Paramedicine 101 is joining up with EMSblogs.com.
We will be moving to www.Paramedicine101.com.
It is still a work in progress right now, but don't hesitate to head over to the new site, because that is where all the new posts will end up.
Thank you for your loyalty as a reader. I hope this doesn't inconvenience you at all.
- Adam Thompson, EMT-P
WE ARE MOVING...
Adam Thompson, EMT-P | 5:56 PM | | 0 comments
Inadequate needle thoracostomy rate in the prehospital setting for presumed pneumothorax: an ultrasound study – abstract
Rogue Medic | 5:27 PM | Critical Judgment, Heresy, Research, Rogue Medic | 1 comments
.jpg)
I have moved Rogue Medic to EMS Blogs. Also posted over at Rogue Medic and at Research Blogging.
Go check out the rest of what is available at EMS Blogs and at Research Blogging.
-
Over at 510 Medic, there is an interesting abstract of a new article on treatment of tension pneumothorax. Frequency of Inadequate Needle Decompression in the Prehospital Setting.
CONCLUSIONS: In this study, 26% of patients who received needle thoracostomy in the prehospital setting for a suspected PTX appeared not to have had a PTX originally, nor had 1 induced by the needle thoracostomy. It may be prudent to evaluate such patients with bedside ultrasound instead of automatically converting all needle thoracostomies to tube thoracostomies.[1]
I have not read the full text.
510 Medic makes some important points and asks some good questions. Then 510 Medic asks -
So if we subscribe to the goal of “first do no harm” and those 15 patients didn’t have a pneumothorax induced by the procedure, is their discomfort worth proper treatment for the remaining 42 patients?[2]
I think that there is a more important question.
Should we assume that the presence of a pneumothorax is an indication for needle decompression?
A pneumothorax is not the same as a tension pneumothorax. Even the definition of a tension pneumothorax is not easy to agree on. I tend to treat with opioids what many others would treat with needle decompression. I have not had any of these patients deteriorate, while in my care. They received chest tubes in the trauma center.
Should we assume that the presence of a pneumothorax is an indication for needle decompression?
57 patients with a prehospital diagnosis of tension pneumothorax. Yes, EMS does diagnose, but that is a discussion for elsewhere. Yes, these patients were diagnosed by EMS with tension pneumothorax, unless we are suspecting acupuncture, because what other prehospital indication is there for sticking a needle into a patient's chest?
Out of 57 patients diagnosed with tension pneumothorax, only 42 patients had a pneumothorax.
How many patients had a tension pneumothorax at the time the needle was stuck into the chest wall?
How many of those patients would have been better off if treated with something other than a needle?
How many complications were there from the needle decompression?
Am I wrong to use italics to highlight the word decompression, since so many of the patients did not have anything to decompress?
We rush to perform procedures that we have little experience with. Isn't this a situation likely to lead to misdiagnosis?
Isn't the infrequent use of needle decompression for suspected tension pneumothorax likely to lead to operator error?
The actual occurrence of tension pneumothorax appears to be much less frequent than the prehospital diagnosis of tension pneumothorax. Isn't that an indication of a failure to properly educate medics?
Footnotes:
[1] Inadequate needle thoracostomy rate in the prehospital setting for presumed pneumothorax: an ultrasound study.
Blaivas M.
J Ultrasound Med. 2010 Sep;29(9):1285-9.
PMID: 20733183 [PubMed - in process]
-
[2] Frequency of Inadequate Needle Decompression in the Prehospital Setting
510 Medic
Article
.
Research: Prehospital Pain Management
Adam Thompson, EMT-P | 9:18 PM | Pharmacology, Research | 1 comments
Check this out...
I'm not sure why IV Fentanyl wasn't compared to Morphine, but the study is interesting none-the-less.
Prehosp Emerg Care. 2010 Oct-Dec;14(4):439-47. [Pubmed]
Effectiveness of morphine, fentanyl, and methoxyflurane in the prehospital setting.
Abstract
Abstract Objective. To compare the effectiveness of intravenous (IV) morphine, intranasal (IN) fentanyl, and inhaled methoxyflurane when administered by paramedics to patients with moderate to severe pain. Methods. We conducted a retrospective comparative study of adult patients with moderate to severe pain treated by paramedics from the Ambulance Service of New South Wales who received IV morphine, IN fentanyl, or inhaled methoxyflurane either alone or in combination between January 1, 2004, and November 30, 2006. We used multivariate logistic regression to analyze data extracted from a clinical database containing routinely entered information from patient health care records. The primary outcome measure was effective analgesia, defined as a reduction in pain severity of >/=30% of initial pain score using an 11-point verbal numeric rating scale (VNRS-11). Results. The study population comprised 52,046 patients aged between 16 and 100 years with VNRS-11 scores of >/=5. All analgesic agents were effective in the majority of patients (81.8%, 80.0%, and 59.1% for morphine, fentanyl, and methoxyflurane, respectively). There was very strong evidence that methoxyflurane was inferior to both morphine and fentanyl (p < 0.0001). There was strong evidence that morphine was more effective than fentanyl (p = 0.002). There was no evidence that combination analgesia was better than either fentanyl or morphine alone. Conclusion. Inhaled methoxyflurane, IN fentanyl, and IV morphine are all effective analgesic agents in the out-of-hospital setting. Morphine and fentanyl are significantly more effective analgesic agents than methoxyflurane. Morphine appears to be more effective than IN fentanyl; however, the benefit of IV morphine may be offset to some degree by the ability to administer IN fentanyl without the need for IV access.
Pain management is one of those things commonly under done by paramedics. I believe common reasons for this lack of treatment include laziness, apathy, and disbelief. Paramedics don't want to do the added paperwork that goes with administering a controlled substance. They may not care too much about the pain that their patient is in, and are much more concerned about life-threatening conditions. Finally, the existence of drug seekers most-definitely decreases the amount of pain meds administered prehospitally. Whatever the reason, it isn't a good one. If your patient complains of pain, it should be treated. An ice pack or positioning may be enough for some, while heavy doses of potent narcotics may be required for others. We have the tools, now lets use them.
I have added the Wong-Baker 'faces' pain scale here to remind you of how to judge your pediatric patient's pain. The old one through ten severity scale is suffice for adults.
Learn It: Angioedema
Adam Thompson, EMT-P | 1:54 PM | Clinical Discussion, Education, Pharmacology, Toxicology | 5 comments
Fire & EMS Blogger Warning: Righthaven Lawsuits
Star of Life Law | 10:23 AM | | 0 comments
Also posted at Star of Life Law.
Fellow Fire and EMS bloggers, if you have not heard of Righthaven, LLC, you might be soon. In the name of a federal copyright lawsuit. Here is what you need to know:
1. Righthaven, LLC is a Las Vegas company established to sue bloggers who clip news content. Most newspapers firmly request bloggers or aggregators take down infringing content and link back to the paper. By comparison, Righthaven goes directly to suing, without any request to take down.
2. Righthaven has issued more than 100 lawsuits since its inception. See Righthaven Victims. See also Righthaven Lawsuits.
3. Righthaven's first client was Nevada-based Stephens Media. The Las Vegas Review Journal is Stephens’ flagship.
4. Righthaven has just struck a deal with Arkansas-based WEHCO Media to expand its copyright litigation campaign, in which bloggers and aggregators across the country are being sued on allegations of infringement. WEHCO controls 28 papers, including the Arkansas Democrat-Gazette in Little Rock, and 13 cable stations largely in the south.
5. Go here for a complete list of Righthaven-owned domains and newspapers.
6. Go here for a Firefox add-on that will prevent you from accessing Righthaven-owned content.
7. From Clayton Cramer, The Armed Citizen, a Righthaven lawsuit victim:
"For those who think that this could be settled out of court cheaply: think again. Other defendants who have approached Righthaven without a lawyer to settle this matter have been told variously, "$7500" or "low five figures" for a single newspaper article infringement."
8. Here is some guidance on how to properly cite news articles on your blog. Post the headline of the story and then the first paragraph with a link to the original story. Like this:
Jogger was listening to iPod when plane hit him, coroner says
The (Hilton Head) Island Packet
Tuesday, Mar. 16, 2010
A Georgia man was running and listening to his iPod on the beach on Hilton Head Island when he was killed by an airplane that made an emergency landing Monday near Palmetto Dunes, the Beaufort County Coroner's Office said today.
The rest of the article can be viewed by clicking here.
Hat tip to Ryan Giles.
9. Police your site. Remove or update potentially infringing posts. Properly cite and link to news sources.
10. If you are a Fire/EMS blogger and get served with a Righthaven lawsuit, feel free to email me.
Drug Shortages Affect Those Still in the Dark Ages – Furosemide
Rogue Medic | 8:24 PM | Medical Mythology, Research, Rogue Medic | 2 comments
.jpg)
I have moved Rogue Medic to EMS Blogs. Also posted over at Rogue Medic and at Research Blogging.
Go check out the rest of what is available at EMS Blogs and at Research Blogging.
-
In the current JEMS, there is an embarrassing article. Drug Shortage Possible in N.Y.
It seems that the drugs that people are worried about are lidocaine, furosemide, 50% dextrose, and epinephrine 1:10,000 preloaded syringes. Here, I will discuss furosemide.
Furosemide is not appropriate for EMS patients, because there are more appropriate drugs, more appropriate other treatments, and it is too often given to patients who have pneumonia.
MANAGEMENT OF APE
Fluid accumulation in the lungs associated with APE, until recently, was attributed to excess accumulation of total body fluid. Accordingly, treatment of APE was aimed at removing excess fluid from the lungs by promoting massive diuresis. However, this explanation for APE could not reconcile the fact that APE typically occurs during early morning hours when fluid intake is minimal. The current explanation is that APE results from fluid redistribution within the body whereby a part of the intravascular volume is redistributed to the lungs as a consequence of increased intravascular pressure as outlined above.13 Primary objectives for the treatment of acute CHF are to reduce pulmonary capillary pressure, to redistribute pulmonary fluid, and to improve forward flow.12,13 These may be achieved by reducing LV preload and afterload, providing ventilatory and inotropic supports, and identifying and treating the underlying etiology of the syndrome (Table 3). It should be recognized that these treatment measures are intended for APE patients who are normotensive or hypertensive and not those who are hypotensive. The latter comprises cardiogenic shock secondary to severe LV systolic dysfunction; treatment of these critically ill patients is beyond the scope of this review.[1]
That is a big paragraph, but there is a lot of information in there. Enough to convince us that we should not be using furosemide to treat an acute onset/exacerbation of heart failure.
In the chart below, before furosemide in treatment there are plenty of other treatments. Notice that only oxygen comes before NTG (NiTroGlycerine) and the more severe the symptoms, the more NTG is given.
Mild symptoms - One 0.4 mg NTG spray/tab - repeated every 4 to 5 minutes.
Moderate symptoms - High-dose NTG, which is explained below.
Severe symptoms - Two to five 0.4 mg sprays/tabs at a time - repeated every 3 to 5 minutes.
But, but, but, but, but, . . . . . we can only give a maximum of 3 NTG - ever.
Then you need to get a better medical director, because your medical director has you killing patients.
Am I being too subtle?
Another treatment that is very effective is CPAP (Continuous Positive Airway Pressure) which is a BLS (Basic Life Support) skill, except where medical directors like to kill patients. When using CPAP (a form of NIPPV - Non-Invasive Positive Pressure Ventilation), NTG paste can be applied. Do not be shy with the paste, because nothing is absorbed well through the skin when the skin is pale. Pale means a lack of circulation. Also, since the appropriate dose is much more than standard NTG dosing, there is not much reason to hold back.
I disagree about the placement of CPAP at the bottom. CPAP should be started right away. This was published in 2003, so it is kind of old and conservative.
You call that NTG use conservative?!?!?
I do. I have given dozens of NTG in a period of 10 to 20 minutes and never had a patient experience any adverse effects while in my care or at the hospital. I have written elsewhere about the superstitious way we approach NTG.
Furosemide is in there, but only if the patient has peripheral edema. If there is no peripheral edema, is fluid overload the problem? That is a fluid redistribution problem. There is fluid in the wrong place, but that does not mean that the whole body is overloaded with fluid or that putting a bunch of fluid in the bladder is going to make things better. Moving fluid to the bladder does not mean that we are removing it from the lungs any more than we are removing fluid from anywhere else.

Click on the chart to make it bigger. I know I can't read any of it at this size. This is from the same paper as the paragraph above.
Well, that is just one paper. Nobody else would be so irresponsible as to recommend such large doses of NTG.
Then let's read about what they do in the ED (Emergency Department).
Most patients who experience CPE, however, do not have ECG evidence of an acute dysrhythmia or AMI. Treatment should therefore be aimed at redistributing the excessive pulmonary interstitial fluid into the systemic circulation, which improves alveolar oxygen-carbon dioxide exchange and hypoxia; therefore, pharmacologic agents that provide preload reduction and afterload reduction should be administered. In some cases, inotropic support is required also.[2]
What drugs do we use to provide preload reduction and afterload reduction?
Nitroglycerin
The most effective and rapidly-acting preload-reducing medication is nitroglycerin (NTG) [21–25]. Multiple studies have demonstrated the superiority of NTG over furosemide [21,24,26–28] and morphine sulfate [28–30] for preload reduction, symptomatic improvement, and safety. NTG can be administered in sublingual, IV, or transdermal form, although the transdermal absorption can be erratic in the patient in extremis. NTG also has the benefit of a short half-life; therefore, if the patient develops a precipitous fall in blood pressure (generally uncommon in CPE {Cardiogenic Pulmonary Edema} patients), the blood pressure should return to previous values within 5 to 10 minutes of discontinuation of administration.[2]
But what about the dose?
In one study [26], 3 mg IV boluses of NTG were administered every 5 minutes to patients who had developed CPE, a dose equivalent to a 600 mg/min infusion. This protocol was found to be safe, well-tolerated, and effective for these patients and associated with reduced need for mechanical ventilation and more rapid resolution of symptoms. Standard anti-anginal dosages of sublingual NTG with which most physicians are comfortable (ie, 400 µg every 5 minutes), has the bioequivalence of an IV NTG infusion of 60 to 80 µg/min. Physicians should, therefore, be comfortable with the safety of even higher dosages of NTG for patients who experience CPE and usually present in a hyper-adrenergic state with moderately-to-severely elevated blood pressures.[2]
That is 7 1/2 times to 10 times the standard dose of NTG - with no problems.
Maybe that maximum of 3 NTG is something that should be ignored. The AHA (American Heart Association) seems to be ignoring it. Just try to find a limit on NTG administration in the current ACLS, which is from 2005.
These papers are available in PDF format, so you can print them out and hand them to your medical director and/or to the other doctors in the ED.
These are important papers. Both are review articles. One is written for EMS, while the other is written for the ED.
If you are feeling aggressive, maybe you can write on the bottom, Call me about improving the protocols we use to treat our patients.
There is one problem with this. This will lead to fewer intubations.
The best intubation is the intubation that is prevented by excellent patient care.
-
Footnotes:
[1] Prehospital therapy for acute congestive heart failure: state of the art.
Mosesso VN Jr, Dunford J, Blackwell T, Griswell JK.
Prehosp Emerg Care. 2003 Jan-Mar;7(1):13-23. Review.
PMID: 12540139 [PubMed - indexed for MEDLINE]
Free Full Text PDF
-
[2] Modern management of cardiogenic pulmonary edema.
Mattu A, Martinez JP, Kelly BS.
Emerg Med Clin North Am. 2005 Nov;23(4):1105-25. Review.
PMID: 16199340 [PubMed - indexed for MEDLINE]
Free Full Text PDF
.
EMS Educast Episode 67
Adam Thompson, EMT-P | 7:11 PM | Education, EMS EduCast, General Discussion | 0 comments
Greg Friese from EMS Educast invited me to guest cohost on episode 67. On the show was David Page from the St. Paul EMS Academy.
Make sure to go check it out.
Thanks for stopping by,
Adam Thompson, EMT-P
Drug Shortages Affect Those Still in the Dark Ages – Lidocaine
Rogue Medic | 6:06 PM | Medical Mythology, Research, Rogue Medic | 2 comments
.jpg)
I have moved Rogue Medic to EMS Blogs. Also posted over at Rogue Medic and at Research Blogging.
Go check out the rest of what is available at EMS Blogs and at Research Blogging.
-
In the current JEMS, there is an embarrassing article. Drug Shortage Possible in N.Y.
It seems that the drugs that people are worried about are lidocaine, furosemide, 50% dextrose, and epinephrine 1:10,000 preloaded syringes. Here, I will discuss lidocaine.
Lidocaine is not appropriate for EMS patients, because there are more appropriate drugs. Lidocaine is still used for cardiac arrest, even though there is absolutely no reason to believe that it does anything positive for the patient.
There is no evidence that any antiarrhythmic drug given routinely during human cardiac arrest increases survival to hospital discharge. Amiodarone, however, has been shown to increase short-term survival to hospital admission when compared with placebo or lidocaine.[1]
In other words, amiodarone doesn't work, but lidocaine is even worse.
-
Lidocaine is also used for ventricular tachycardia
 with similar lack of effect.
with similar lack of effect.Lidocaine terminated ventricular tachycardia in four of 31 patients, ajmaline in 19 of 30 patients (P<0.001).[2]
Lidocaine is no better than holding the patients hand or any other placebo. Spontaneous remission of ventricular tachycardia should occur in more than 4 out of 31 patients.
DC shock was used in 16 nonresponders (22.9%) to procainamide and 10 non-responders (50%) to lidocaine.[3]
Only 35% of patients improved after lidocaine. Maybe they improved because of lidocaine - maybe not. More important is that 50% of patients who received lidocaine ended up being cardioverted. Did they require cardioversion because of the lidocaine?
Would you recommend a drug that leads to half of patients being cardioverted?
-
Footnotes:
-
[1] Medications for Arrest Rhythms
2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care
Part 7.2: Management of Cardiac Arrest
Free Full Text
-
[2] Electrophysiological and haemodynamic effects of lidocaine and ajmaline in the management of sustained ventricular tachycardia.
Manz M, Mletzko R, Jung W, Lüderitz B.
Eur Heart J. 1992 Aug;13(8):1123-8.
PMID: 1505562 [PubMed - indexed for MEDLINE]
-
[3] Efficacy of procainamide and lidocaine in terminating sustained monomorphic ventricular tachycardia.
Komura S, Chinushi M, Furushima H, Hosaka Y, Izumi D, Iijima K, Watanabe H, Yagihara N, Aizawa Y.
Circ J. 2010;74(5):864-9. Epub 2010 Mar 26.
PMID: 20339190 [PubMed - indexed for MEDLINE]
Free Full Text PDF
Table 3 is from this paper. As you can see, lidocaine is a joke compared to procainamide.
.
Church of the Blog O Sphere: EMS Garage Episode 99
Rogue Medic | 12:32 PM | EMS Garage, Rogue Medic | 2 comments
.jpg)

Also posted over at Rogue Medic. I have moved to EMS Blogs. Go check out the rest of what is there.
On the most recent EMS Garage - Church of the Blog O Sphere: EMS Garage Episode 99, we spent a bit of time discussing how to persuade people that we should change things and how we can determine what is the truth.
Listen to the show.
.
Need Your Help
Adam Thompson, EMT-P | 4:45 PM | General Discussion | 3 comments
I am looking for help with the following projects:
- Paramedicine 101 Podcast
- Interactive Educational Software
I am also looking for software developers to assist me with the creation of something I have been working on. It would be an interactive presentation/educational program. Assistance with this would gain you commission on any income made.
Last but not least. I am looking for an artist/illustrator. Someone, preferably with experience illustrating the human anatomy.
Contact Adam Thompson at Paramedicine101@gmail.com
McLearning and 12-Lead ECG interpretation
Tom B | 12:16 PM | | 5 comments
I've been giving a lot of thought lately to paramedic education and the problem of 12-lead ECG interpretation.
Specifically, the reasons why paramedics aren't taught to actually read a 12-lead ECG and are instead given a crash course in "STEMI recognition" which does not prepare the student to differentiate between the ST-elevation of acute STEMI and other causes of ST-elevation.
This TED Talk by Dan Meyer about high school math education struck a chord with me. I highly recommend the entire talk, but the most relevant part for this discussion starts at 01:50.
Here's the part that really resonated with me:
"David Milch, creator of Deadwood and other amazing TV shows [...] swore off creating contemporary drama -- shows set in the present day -- because he saw that when people filled their minds with 4 hours a day of, for example, 2 1/2 Men, it shapes the neuro-pathways in such a way that they expect simple problems. He called it an "impatience with irresolution". You're impatient with things that don't resolve quickly. You expect sitcom-sized problems that wrap up in 22 minutes, 3 commercial breaks and a laugh track.
I'll put it to all of you -- what you already know. No problem worth solving is that simple."
Doesn't that exactly describe the paramedic approach to 12-lead ECG interpretation?
EKGs for Dummies, 12-Leads Made Easy, Rapid STEMI ID, etc. etc. etc.
Just the "need to know" information without all the difficulty of axis determination, bundle branch blocks, electrolyte derangements, differential diagnosis of tachycardias, primary and secondary ST-T wave abnormalities, identifying acute STEMI in the presence of STE-mimics, and other things that we have no patience for because we can't learn it in 22 minutes.
As if we can jump straight to the finish line and enjoy the fruits of victory without ever preparing for the race.
The problem is compounded by policy makers who "don't know what they don't know" (thank you Don Rumsfeld). They consider it a foregone conclusion that comprehensive 12-lead ECG knowledge is not practical for paramedics.
I say that it's indispensable.
Show Me Your Rig
Adam Thompson, EMT-P | 10:28 AM | General Discussion | 0 comments
On the Paramedicine 101 Facebook page, I am asking the readers to show off their ambulance. Maybe we can get to know each other a little by gawking at the trucks we drive. Go post a picture of your chariot.
Research: Management of the Airway in the Trauma Patient
Adam Thompson, EMT-P | 5:55 PM | Aeromedical, Airway, Airway Management, Intubation, Research, Trauma | 1 comments
Check this out...
J Trauma. 2010 Aug;69(2):294-301. [Pubmed]
Prehospital airway and ventilation management: a trauma score and injury severity score-based analysis.
Davis DP, Peay J, Sise MJ, Kennedy F, Simon F, Tominaga G, Steele J, Coimbra R.
Abstract
BACKGROUND:: Emergent endotracheal intubation (ETI) is considered the standard of care for patients with severe traumatic brain injury (TBI). However, recent evidence suggests that the procedure may be associated with increased mortality, possibly reflecting inadequate training, suboptimal patient selection, or inappropriate ventilation. OBJECTIVE:: To explore prehospital ETI in patients with severe TBI using a novel application of Trauma Score and Injury Severity Score methodology. METHODS:: Patients with moderate-to-severe TBI (head Abbreviated Injury Scale score 3+) were identified from our county trauma registry. Demographic information, pre-resuscitation vital signs, and injury severity scores were used to calculate a probability of survival for each patient. The relationship between outcome and prehospital ETI, provider type (air vs. ground), and ventilation status were explored using observed survival-predicted survival and the ratio of unexpected survivors/deaths. RESULTS:: A total of 11,000 patients were identified with complete data for this analysis. Observed and predicted survivals were similar for both intubated and nonintubated patients. The ratio of unexpected survivors/deaths increased and observed survival exceeded predicted survival for intubated patients with lower predicted survival values. Both intubated and nonintubated patients transported by air medical crews had better outcomes than those transported by ground. Both hypo- and hypercapnia were associated with worse outcomes in intubated but not in nonintubated patients. CONCLUSIONS:: Prehospital intubation seems to improve outcomes in more critically injured TBI patients. Air medical outcomes are better than predicted for both intubated and nonintubated TBI patients. Iatrogenic hyper- and hypoventilations are associated with worse outcomes.
This publication is prestigious enough to trust the validity of the study. It looks as if enough patients were ruled-in to take consideration of the evidence. With the increase in ICP (intracranial pressure) that intubation causes, it has been theorized in the past, that intubating the TBI patient only made them worse. However, this study shines a different light. So what do you think? The discussion is open.
I am not a cretin
Adam Thompson, EMT-P | 8:06 AM | General Discussion | 0 comments
Back during EMS Week, EMS1.com held a writing contest. Kelly Grayson, AKA Ambulance Driver called on us EMS bloggers to make submissions. The theme was Anytime, Anywhere, We'll be there. I am not sure who one, but the top 6 can be seen here. Below is my submission. Enjoy...
I am not a cretin
Names and events have been altered to protect the patient's privacy.
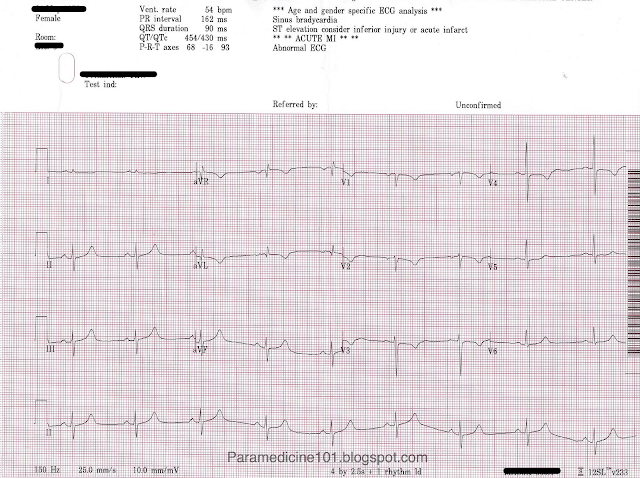
ECG: 40 y/o Female with Chest Pain
Adam Thompson, EMT-P | 10:49 PM | Case Reviews, ECG/EKG Archive | 26 comments
Also Posted over at ECG Experts
Submission thanks to Tim Waters, CCEMTP of Lee County Medstar
40 yo female, thin build with no history/meds/allergies. + smoker. Works as painter outside and was painting when developed pain in her upper chest/left arm which is the same she uses to paint. Also adds that she has been moving and lifting numerous heavy objects over the past week and since then has been having these episodes of shoulder discomfort. Pain is non-radiating with moderate reproducibility with movement and inspiration. I forget what severity scale she gave it but was definitely uncomfortable. Onset was about 3 ½ hours prior to presentation while painting with her trying to work through the pain until it became to unbearable.. Denies nausea, is diaphoretic but has been working outside.
#CoEMS: CPR Effectiveness
Adam Thompson, EMT-P | 6:29 PM | Cardiac Arrest, Cardiocerebral resuscitation, CoEMS, Education, EMS 2.0 | 0 comments
Chronicles of EMS, A Seat at the Table takes on CPR effectiveness. The Las Vegas video that they mention can be found below as well. Keep up the good work Justin and Mark!
Side note - ILCOR, The International Liaison Committee On Resuscitation has not found any supporting evidence for the Autopulse. They are the ones whom do the research for AHA. Also, transporting patients without a pulse should be re-looked at by any agency performing this practice. The initial treatment at the ER will not differ from the treatment we provide at the scene per ACLS guidelines. Why not give the patient the best chance possible. If they don't get a pulse back on scene, it is probably never going to come back--that's just the facts.
Product Review: AHA's Rapid STEMI ID
Adam Thompson, EMT-P | 11:07 AM | Cardiology, Education, Product Review | 2 comments
- Rate & Rhythm
- Axis determination
- Complex, wave, and segment durations
- Morphology
- STE-Mimics
- Ischemia, Injury, Infarct
Research: Management of the Airway in the Burn Patient
Adam Thompson, EMT-P | 10:44 AM | Airway, Airway Management, Intubation, Research | 3 comments
Check this out...
J Burn Care Res. 2010 Jul 14. [Epub ahead of print]
Pre-Burn Center Management of the Burned Airway: Do We Know Enough?
Eastman AL, Arnoldo BA, Hunt JL, Purdue GF.
Abstract
Despite the traditional teaching of early and aggressive airway management in thermally injured patients, paramedics and medical providers outside of burn centers receive little formal training in this difficult skill set. However, the initial airway management of these patients is often performed by these preburn center providers (PBCPs). The purpose of this study was to evaluate the authors' experience with patients intubated by PBCPs and subsequently managed at the authors' center. A retrospective review of a level I burn center database was undertaken. All records of patients arriving intubated were reviewed. From January 1982 to June 2005, 11,143 patients were admitted to the regional burn center; 11.4% (n = 1,272) were intubated before arrival. In this group, mean age was 37.1 years, mean burn size was 35.3% TBSA, and mean length of hospital stay was 27.0 days. Approximately 26.3% were suspected of having an inhalation injury, and this was confirmed by either bronchoscopy or clinical course in 88.6% of this subgroup. Mortality in patients arriving intubated was 30.8%, and these were excluded from the rest of the analysis. In the surviving 879 intubated patients, reasons reported by PBCPs for intubation included "airway swelling" in 34.1%, "prophylaxis" in 27.9%, and "ventilation or oxygenation needs" in 13.2%. Of these patients, 16.3% arrived directly from the scene, with the remainder arriving from another hospital facility. Of all survivors who arrived intubated, 11.9% were extubated on the day of admission, 21.3% were extubated on the first postburn day (PBD), and 8.2% were extubated on the second PBD. No patients who were extubated on PBD1 or PBD2 had to be reintubated. A significant number of burn patients have their initial airway management by PBCPs. Of these, a significant number are extubated soon after arrival at the burn center without adverse sequelae. Rationale for their initial intubation varies, but education is warranted in the prehospital community to reduce unnecessary intubation of the burn patient.
Any thoughts or input?
How can we better educate our selves and fellow prehospital providers on this topic?
Research: Prehospital Thrombolysis
Adam Thompson, EMT-P | 1:00 PM | Cardiology, Clinical Discussion, Research | 0 comments
Check this out...
Also a topic within The EKG Club
Emerg Med J. 2010 Aug 3. [Epub ahead of print]
Paramedic decision making: prehospital thrombolysis and beyond.
Smith AM, Hardy PJ, Sandler DA, Cooke J.
Abstract
Background Mortality from acute myocardial infarction is influenced by the speed at which reperfusion therapy is delivered. In the UK, prehospital thrombolysis (PHT), administered by paramedics, has been developed to improve call to needle (CTN) times. Recently, it has been shown in randomised trials that mortality can be further reduced by primary percutaneous coronary intervention (PPCI). This project was developed to assess current ST-elevation myocardial infarction practice in a district general hospital and to prepare paramedics for PPCI. Methods Data were collected prospectively over a 12-month period for all patients who received thrombolysis for a presumed myocardial infarct. The primary outcome measures for each case were who delivered the thrombolysis, either the paramedic crew or the hospital, and if the patient did not receive PHT the reason why not. Secondary outcome measures included the CTN time. Results 153 patients received thrombolysis over the time period (99 men, 54 women, mean age 66+/-15 years). Of this group, 55 patients received PHT (35.9%) with a median CTN time of 36 min (inter-quartile range (IQR) 30-42 min). The commonest reason for exclusion from receiving PHT was that the patient's history did not fit the eligibility criteria (25% of cases). Conclusions Paramedics are able to deliver PHT promptly and safely. With the focus now on PPCI, it is anticipated that not only will paramedics be able to select patients for delivery to a heart attack centre for PPCI, they will be selecting many more patients for this treatment than have up to now received PHT.
So, what do you think? Are you ready to start administering clot busters? Here is another abstract that concludes that the early identification of STEMI improves patient outcomes.
Am J Cardiol. 2009 Apr 1;103(7):907-12. Epub 2009 Feb 7.
Effect of prehospital triage on revascularization times, left ventricular function, and survival in patients with ST-elevation myocardial infarction.
Sivagangabalan G, Ong AT, Narayan A, Sadick N, Hansen PS, Nelson GC, Flynn M, Ross DL, Boyages SC, Kovoor P.
Abstract
Shorter reperfusion times lead to better outcomes in patients with ST-elevation myocardial infarction (STEMI). We assessed the efficacy of prehospital triage with bypass of community hospitals and early activation of the cardiac catheterization team on revascularization times, left ventricular (LV) ejection fraction, and survival. Patients with STEMI (624) were divided into 3 groups determined by site of triage: ambulance field triage (163), interventional center emergency department (202), and 3 community hospital emergency departments (259). Compared with community hospital and interventional center triages, ambulance field triage resulted in a significant median decrease in door-to-balloon times of 68 and 27 minutes, respectively (p <0.001). LV ejection fraction was highest in the field triage group (52 +/- 13%) compared with the interventional center (49 +/- 12%) and community hospital (48 +/- 12%, p = 0.017) groups. Thirty-day mortality was lowest in the ambulance field group (3%) compared with the interventional facility (11%) and community hospital (4%, p = 0.007) groups. There was a significant difference in long-term survival with up to 30-month follow-up among the 3 triage groups (p = 0.041). With time-dependent Cox regression modeling the difference in survival was significant only during the first week after STEMI (p = 0.020). Every extra minute of symptom onset to reperfusion time was associated with a relative risk of long-term mortality of 1.003 (95% confidence interval 1.000 to 1.006, p = 0.027). In conclusion, field triage of patient with STEMI decreased revascularization times, which preserved LV function, and improved early survival.And another advocating statement from 2007:
J Emerg Med. 2008 May;34(4):405-16. Epub 2007 Dec 27.
The role of fibrinolytics in the prehospital treatment of ST-elevation myocardial infarction (STEMI).
Sayah AJ, Roe MT.
Abstract
The efficacy of fibrinolytics in the treatment of ST-elevation myocardial infarction is directly related to the time of administration, with the first 2 h after symptom onset seen as a critical period for greatest improvement in cardiovascular parameters and mortality. The American College of Cardiology/American Heart Association recommends a medical contact to treatment time of 30 min for fibrinolysis in patients with ST-elevation myocardial infarction. In selected patients, reperfusion goals may be expedited with prehospital administration of fibrinolytics. In clinical trials, prehospital fibrinolysis markedly reduced the time from symptom onset to treatment, allowed earlier ST-segment resolution, and reduced short- and long-term mortality compared with in-hospital treatment. Prehospital fibrinolysis has become more feasible with the introduction of prehospital 12-lead electrocardiography, improved skills of emergency medical services personnel, improved communication with the Emergency Department, and the advent of bolus fibrinolysis. Rapid and accurate administration of a fibrinolytic is vital for the success of prehospital fibrinolysis.
Okay, that one is a bit old. Lets open the discussion on this topic. Let me know what you think. Provide some better research, and I will tell you now... there is some out there. I'd also like to hear from anyone out there that has been a part of a thrombolysis trial.
Thanks for your participation,
Adam Thompson, EMT-P
Research: Pediatric Pain Management
Adam Thompson, EMT-P | 10:28 PM | Clinical Discussion, Research | 7 comments
Check this out...
Am J Emerg Med. 2010 Aug 2. [Epub ahead of print]
Out-of-hospital emergency medicine in pediatric patients: prevalence and management of pain.
Galinski M, Picco N, Hennequin B, Raphael V, Ayachi A, Beruben A, Lapostolle F, Adnet F.
Abstract
INTRODUCTION: Much less is known about pain prevalence in pediatric patients in an out-of-hospital than emergency department setting. The purpose of this study was to determine pain prevalence in children in a prehospital emergency setting and to identify the factors associated with pain relief. MATERIALS AND METHODS: This prospective cohort study in consecutive patients 15 years or younger was conducted by 5 mobile intensive care units working 24/7 (January-December 2005). The presence of pain, its intensity, and alleviation by the administration of analgesics were recorded. RESULTS: A total of 258 of 433 pediatric patients were included, of whom 96 were suffering from acute pain (37%; 95% confidence interval [CI], 31-43) that was intense to severe in 67% of cases. Trauma was the only factor significantly associated with acute pain (odds ratio, 818; 95% CI, 153-4376). Overall, 92% of the children in pain received at least one analgesic drug; 41% received a combination of drugs. Opioid administration was significantly associated with intense to severe pain (odds ratio, 7; 95% CI, 2-25). On arrival at hospital, 67% of the children were still in pain; but 84% had experienced some pain relief regardless of their sex, age, or disorder. CONCLUSION: In a prehospital emergency setting, more than a third of children experience acute pain with a high prevalence of intense to severe pain. Scoring pain in children, and especially in the newborn, is beleaguered by a lack of suitable scales. Despite this, it was possible to treat 90% of children in pain and provide relief in 80% of cases.If we could only get these numbers with our adult patients. I can't help but believe this is due to a couple main factors. 1. We inherently want to make kids feel better & 2. We are pretty sure that our pediatric patients aren't drug seekers.
Here is some advice, treat adult patience that have pain as if they were pediatric patients that have pain. Just make sure you adjust the dose proportionately. This is not an attempt to be cynical, yet just the opposite. I am attempting to remove all cynical notions preventing appropriate pain management.
Grand Rounds - 3
Adam Thompson, EMT-P | 10:51 AM | | 0 comments
The August edition of Grand Rounds is now up over at EMSResponder.com. Click here to check it out.
Peter Pronovost - The Science of Safety
Tom B | 2:19 PM | | 0 comments
As some of you may know, Crew Resource Management is an area of interest for me.
Advocating Airway Education
Adam Thompson, EMT-P | 7:13 PM | Airway, Airway Management, Education, Intubation | 9 comments
In the popular and acclaimed JEMS article Experts Debate Paramedic Intubation, there were a few key points made that I would like to elaborate on, as well as provide some of my own insight from the research I have come across.
Key Point 1
Experience should be maintained in a number of manors:
- Operating room rotations
- Mannequin scenarios (without the dummy supine on a table)
- Cadavers if possible
Dr. Bledsoe: Do you feel there’s a role for RSI in the prehospital setting? Dr. Wayne, I know your program has decades of success with RSI. What do you think?
Dr. Wayne: Although there are no nationally defined indications for the use of RSI in the field, we at Whatcom Medic One believe that RSI is indicated for any patient in whom there’s a need to control an “uncontrolled” airway. This may include depressed GCS score, excess secretions, hypoxia that may be correctable, ventilatory fatigue or central nervous system depression with or without secondary respiratory depression.
Dr. Tan: I believe there is, but it must be in the right context with requisite oversight and extraordinary training. I oversee more than 100 paramedics in my system, yet only 10 of them have RSI privileges. They’re required to obtain critical care certification, attend ongoing training sessions with me every 12 weeks, attend annual specialized training courses and undergo 100% audits of their critical care trips. It’s a strenuous and time-consuming process but one that can’t be overemphasized given the complexity and danger inherent to RSI. I certainly don’t believe RSI should be a “routine” part of any standing orders, as there is nothing routine about it.
Dr. Wang: I think RSI should be restricted to the aeromedical setting for use by critical care flight nurses and/or flight medics for the reasons I’ve previously detailed. I really challenge those medical directors who currently allow RSI and promote its use in other systems. Although I applaud their efforts and attention to quality improvement and training, they still equate successful intubation with a positive outcome. As Dr. Eckstein said, in the absence of prospective RCTs, we can’t assume that prehospital RSI has actually improved outcomes for our patients.
Dr. Eckstein: RSI is potentially useful where paramedics have exceptional skill, training and medical oversight. Unfortunately, this is a tiny fraction of EMS agencies. If we replaced the “I” (intubation) with “A” (airway—Combitube, King, etc.), this might relieve much of the angst over prehospital RSI.
- Is there a risk for aspiration?
- Is the patient ventilating on their own?
- Is the patient oxygenating on their own?
- Is the patient conscious?
- How difficult will this ETI attempt be?
- What is my backup plan?
- Bag-valve mask (possibly with an OPA/NPA)
- Combi-tube
- King LT/LTD
- Laryngeal Mask Airway
Dr. Bledsoe: Are the alternative airway devices (e.g., King LT, etc.) good enough for prehospital airway management?
Mr. Gandy: Yes. The studies have shown that excellent ventilation can be achieved with these devices.
Key Point 3
Mr. Gandy: The biggest problem is inadequate training and practice in airway evaluation, such as using the Malampatti or Cormack-Lehane criteria; using aids to intubation, such as bougies; the BURP maneuver; alternative laryngoscope techniques, such as the “skyhook” technique; and a good assortment of alternative airway devices, including either GlideScope or AirTraq. Ventilation should be emphasized over intubation, and extensive practice with BVM ventilation should be required.
Malampatti scoring is done by having the patient stick out their tongue. The difficulty of the proceeding ETI attempt can be gauged by the visibility of the oropharynx.
Cormack-Lehane Citeria is utilized with direct laryngoscopy. This is done by visualizing the vocal cords and making note of how much of the opening is visible:
- Grade 1, visualization of the entire laryngeal aperture;
- Grade 2, visualization of parts of the laryngeal aperture or the arytenoids;
- Grade 3, visualization of only the epiglottis; and
- Grade 4, visualization of only the soft palate.
BURP Maneuver - Backward, Upward, Rightward, Pressure of the larynx.
Don't worry if you don't understand the picture above. It is just a step by step of the BURP maneuver. Basically you place your fingers on the palpable cricoid ring of the patient. Push towards their posterior, and slightly towards their right. This should bring the trachea and it's structures to the best point of view during direct laryngoscopy.
"Skyhook" - I believe Gandy is referring to what my peers and I call the "fish hook" maneuver. This is reserved for the more hefty patients that may be hard to intubate.
This is a two person procedure. One person is dedicated to laryngocopy, and the other will direct person 1, visualize the vocal cords, and pass the ET tube.
Person 1 - With Laryngoscope and a Macintosh blade
- Straddle the supine patient
- Hook the blade into the mouth
- Pull back, keeping the blade off of the teeth
- Make adjustments based off person 2's direction
Person 2 - With appropriately sized ET Tube
- Position yourself at patient's head
- Direct person 2 until the vocal cords are visible
- Pass ET tube
I spoke about the Glidescope in my post Video Laryngocopy. Go check it out.
Key Point 5