I posted this article over at http://www.lifeunderthelights.com/ a few days ago and I thought it would good for here as well. I'm sorry that I've only rarely posted here, but I read this blog quite often and recommend it to all of my peers. Enjoy
-----------------------------------------------
A few years ago I responded to a structure fire on the main engine out of my station. The fire was at a house that had been converted to a dog kennel and grooming shop just a few blocks away from the firehouse and was a short response time. It was a light-staffing day and we responded as a three person engine company. As the senior firefighter I was the acting company officer and my new girlfriend at the time, who just happens to be my wife now, was the backseat firefighter. Get ready for the “Awwww” moment… it was our first fire “as a couple”. There was a number of cool things that came out of the fire, but one of them was the fact that Gina grabbed *my* maul.
On our main engine, there’s an 8-pound maul (big hammer) that I grab as my tool of choice every time I jump off the truck for a fire. It just tucks so neatly in my SCBA’s belt and is so compact yet handy that I make a beeline for it every time. This time, Gina had taken it, so I grabbed a pick-head axe.
It’s amazing when I have my maul how every access problem looks like something that I can solve by whacking it with a hammer of some sort. On this fire, I learned that when one has an axe, every problem looks like it can be solved by some sort of chopping.
Moral of the story, Gina and I entered the structure, saved the pooches, and stopped the fire in its trucks with minimal damage. There’s actually a hilarious video that I believe is still on our department’s web site that I’d let you see if I didn’t hide the name of the department(s) I work for due to reasons of wanting to remain employed.
And, like a lot of posts I write, I told you that so I could tell you this about an EMS call I responded to an indeterminate amount of time ago. I have the honor and privilege to be the senior medic on most shifts I work and I precept a lot of students on the ambulance. This shift was no different and this 0-dark-30 call illustrates a point that I’d like to explain to you.
For this call, the primary ambulance out of our station responded because they were on the way back from another call and my partner and I responded in our ambulance because we were up on the alternating call rotation. They arrived at the poorly-accessible apartment complex a few minutes before we did and made first patient contact. As it turns out, the middle age patient had ran out of his/her prescription Lasix (a potent diuretic, or water pill) a week or so prior to the call and had been retaining a great deal of excess bodily fluid. The patient’s legs were markedly and grossly swollen and weeping fluid out of fluid filled blisters. The Patient called us because he/she could no longer stand the pain of the cellulitis (infection) that had developed. The patient had no respiratory compromise, his/her lungs were clear, and he/she really had no other complaints. The patient had an extensive medical history of organ failure and disease. He/she was fully alert and oriented, and was able to assist us as we simply picked him/her up and carried him/her to the cot.
As we were loading the patient up in the ambulance and I was about to get into the back to continue my assessment and treatment of the patient, the EMT from the other ambulance who happens to be an almost-done Paramedic student told me, “So those legs are the worst I’ve ever seen fluid wise, you’re going to push some lasix on this one”. I mumbled something and got into the truck. I was tired and wasn’t really able to form complete sentences at the time due to sleep deprivation. I continued my assessment where I found that the frail patient had a blood pressure in the 70 systolic range (Low!) and that in addition to retaining fluid in his/her legs, he/she was also retaining fluid in his/her abdomen and was probably in need of a paracentesis. I managed the patient with a (beautifully executed, I must say) IV stick into an impossibly small and crooked vein, and gave just enough fluid to bring his/her BP up a bit without adding to his/her fluid overload all that much. I put the Pt on oxygen and a cardiac monitor, which revealed a normal sinus rhythm without ectopy and obtained a 12-lead EKG as well, which was not indicative of any acute problems. The patient stated that his/her pain was managed by padding and positioning of his/her swollen legs and even though he/she complained of no breathing problems, I put him/her on a bit of oxygen via nasal cannula.
The transport was uneventful, although his/her blood pressure never did come up. The ER later diagnosed the Pt with complete liver failure and toxicity.
But the interesting part of the story is this, when I got back the medic student asked me about giving IV lasix to the patient, as we carry that in our medication stock and have it available as an emergency diuretic for patients in congestive heart failure and/or fluid overload with pulmonary edema and respiratory compromise. He was almost taken aback when I said that I didn’t give any.
I asked him if he did a full assessment. He said that he had tried… but that he didn’t have enough time before I arrived and we took the patient out to the ambulance. I gave him my assessment findings and the news of the very low blood pressure. He said that he agreed with me on not giving the lasix with the markedly low blood pressure but was curious when I explained that it wasn’t the reason I didn’t give the medication.
We in EMS, and especially new providers carry our own hammers… our treatments and medications that we’re able to give in the field. Medics that use these treatments more often are called “aggressive” and it is a badge of honor. In fact, in some cases, aggressive field treatment is indeed warranted and improves patient outcomes. However, in a lot of cases it is not indicated and patients benefit from what we don’t do more so than from what we could have done.
This patient didn’t have any respiratory compromise and while he/she obviously could have benefited from the dieresis or removal of the excess fluid, she didn’t meet the criteria for emergent field administration of lasix, which is respiratory compromise from pulmonary edema. I made the decision to let the physician evaluate the patient and determine the best treatment path that would fit in with the patient’s ultimate plan of care. I didn’t believe that the patient would ultimately benefit from my administration of lasix twenty minutes earlier than the ER could have done it if the physician so chose.
Every treatment we administer must be given with a full assessment of the risks and benefits to the patient for doing so. Every EMS person should familiarize themselves with the long-term care paths of the conditions we treat and try to maximize the long-term benefit to the patient with the acute and short-term care we give. Not every problem is “a nail” and sometimes the hammers we carry aren’t the best ultimate solution for excellent patient care. Remembering how we as EMS people fit into the grand scheme of the overall healthcare system and in the ultimate care paths of our patients will help us all to do what we’re supposed to do, which is to provide excellent and appropriate patient care.
It is also of note, I guess, that Gina rarely steals my maul anymore. Now that we’re married… I “give it freely” to her.. What’s mine is her’s, as they say.
--------------------------------------------
The original post has some pictures of the fire and of the doggies that my wife and I saved on our first "Fire Date" - It can be seen HERE
When All You Have is a Hammer, Every Problem Looks Like... Lasix?
Ckemtp | 8:38 PM | Case Reviews, Clinical Discussion, Critical Judgment, Education, Medical Emergencies, paramedics, Pharmacology | 1 comments
2010 AHA Updates
Adam Thompson, EMT-P | 12:30 AM | Cardiac Arrest, Cardiocerebral resuscitation, EMS News, Research | 2 comments
It's that time again. As most of us Americans in the wide world of emergency medicine know, every five years the American Heart Association updates their recommendations. Those recommendations happen to be the standard for most prehospital agencies, and hospital systems. They say and we do. So what are we going to be doing now?
This year should not be bringing about any mega changes. The direction has stayed the same for the most part.
Where do the updates come from?
ILCOR - The International Liaison Committee on Resuscitation
Process for Evidence Evaluation
The publication of the 2010 International Consensus on Cardiopulmonary Resuscitation (CPR) and Emergency Cardiovascular Care (ECC) Science with Treatment Recommendations (CoSTR) will represent the scientific consensus of experts from a variety of countries, cultures and disciplines. Internationally recognized experts were brought together by the International Liaison Committee on Resuscitation (ILCOR) to evaluate and form an expert consensus on all peer reviewed scientific studies related to CPR.
To achieve this goals, ILCOR is conducting systematic reviews and updates of scientific evidence supporting resuscitation treatment recommendations. More than 500 resuscitation scientific topics will undergo evidence-based review. This process represents the most comprehensive, systematic review of the resuscitation literature to date.
The worksheets posted at this site represent the first step of an international consensus evidence evaluation process that will culminate in the publication of the 2010 International Consensus on CPR and ECC Science with Treatment Recommendations. In addition, resuscitation council-specific guidelines will also be published based on this international science consensus. Worksheet authors and expert reviewers worked very hard to present the information objectively.
The information contained in these worksheets will be presented and discussed between now and early 2010. In early 2010, the International CPR Consensus Conference will convene to allow final presentation and discussion of these worksheets, leading to evaluation and consensus by respective ILCOR Task Forces.
Readers are cautioned that these worksheets are a preliminary review and do not represent any ILCOR Task Force or Resuscitation Council recommendations.
ILCOR recognizes that the integrity of the evidence evaluation process depends on successfully managing real and perceived conflict of interest. ILCOR has policies in place to manage conflict of interest.
The 2010 evidence evaluation and science review process will culminate with the International CoSTR Conference in early 2010, in Dallas, Texas.
A separate publication covering guideline recommendations will be published by each resuscitation council.
So what does this all mean?
The AHA is part of an international committee that uses a systematic review system to scan through all the most valuable research available. The research is graded by how useful an unbiased it is, and then recommendations are made based upon a compilation of the results. The package all of this up in a nice-looking book, packed with a bunch of fancy flow charts, tables, and algorithms, and we buy it.
Link to the questions asked for 2010
Time of old
Amiodarone - Back in 2000 Amiodarone was given a class IIb recommendation from AHA. This was a push from, who else, the manufacturers of Amio. This happened synchronously with the changing of Lidocaine from a class IIb to an indeterminate rating. This occurred after a study showed that Amiodarone improved the number of cardiac arrest that regained pulses. This was accepted by many, and all the better, Amio works in atrial and ventricular arrhythmias--yippee.
The facts:
- Amiodarone improved the amount of people that regained pulses, but not the amount of cardiac arrests that survived to discharge. No more people are surviving on Amio compared to Lidocaine. AHA knows this now, and has known this for a while.
- AHA says that an "indeterminate" rating is no different from class IIb. So why the change? Because class IIb sounds a whole lot better when your selling a new drug.
So does this mean we are going back to lidocaine? Not sure, because there isn't any evidence that lidocaine is any better either--should we confuse everyone more? In fact, there is no evidence that any dysrhythmic does anything beneficial in cardiac arrest. That's right, no quality evidence supporting beneficial effects of dysrhythmics. Want some more? NO DRUGS administered in cardiac arrest have any supporting evidence!
Olasveengen TM, Sunde K, Brunborg C, et al. Intravenous drug administration
during out-of-hospital cardiac arrest. JAMA 2009;302:2222-2229.
Despite the traditional use of intravenous medications such as vasopressors and antiarrhythmics for victims of cardiac arrest, there is actually very little evidence to support these therapies. On the contrary, a recent multicenter center study demonstrated that the use of intravenous medications that are advocated in standard advanced cardiac life support (ACLS) guidelines was ineffective at improving survival of patients with out- of-hospital cardiac arrest (1). Olasveengen and colleagues now add further support to the contention that the use of intravenous medications in victims of non-traumatic cardiac arrest is not associated with improvements in meaningful outcomes. The authors performed a prospective randomized trial of consecutive adults with non-traumatic cardiac arrest that were treated within their emergency medical services (EMS) system in Oslo between 2003 2008. Patients were randomized to either receive standard ACLS therapies with intravenous drug administration (IV group) or ACLS therapies without any intravenous drugs (no IV group). A total of 851 patients were included in the study, 418 patients in the IV group and 433 in the no IV group. The researchers found there was an increase in survival to hospital admission with return of spontaneous circulation in the IV group vs. the no IV group (32% vs. 21%, P < 0.001). However, there was no difference between the IV group vs. the no IV group in terms of survival to hospital discharge (10.5% vs. 9.2%, P = 0.61), survival with favorable neurological outcome (9.8% vs. 8.1%, P = 0.45), or survival at 1 year (10% vs. 8%, P = 0.53). The results demonstrate that with the use of IV ACLS medications, patients simply die in the hospital rather than in the ED. Practically speaking, this amounts to increased intensive care unit bed utilization, hospital resource utilization, and expenses; but without any increase in meaningful survival. In this era of ED and hospital overcrowding and the increasing demand for cost-effectiveness in medical therapies, Stiell’s and Olasveengen’s studies should force us to consider that the use of IV medications for patients in cardiac arrest should be the exception rather than the rule…or guideline.
1. Stiell IG, Wells GA, Field B, et al. Ontario Prehospital Advanced Life Support Study Group. Advanced cardiac life support in out-of-hospital cardiac arrest. N Engl J Med 2004;351:647-656.Back to Amiodarone 2010:
CONSENSUS ON SCIENCE:
Evidence from 1 RCT demonstrates the benefit of amiodarone over placebo for shock refractory or recurrent VT/VF for the endpoint of survival to hospital admission, but not to survival to hospital discharge. Retrospective trials show that lidocaine may be more beneficial than placebo, but selection bias mars these trials. In trials that directly compare amiodarone to lidocaine, patients administered amiodarone generally do better in short term results (ie survival to hospital admission), but no trial has shown an improvement in overall survival (Dorian P 2002 p884, Somberg J 2002 p853).
These trials were performed before the benefits of hypothermia was known, thus they did not incorporate this now proven therapy which improves survival after ROSC. Whether survival to hospital discharge and neurologic survival could be improved with amiodarone and subsequent hypothermia is not known. If that is the case then a stronger argument for amiodarone could be made; if that is not the case then an argument could be made to not give an AAD at all.
CPR Before Defibrillation
It was taught, back in 2005 by AHA, that we need to prime the pump. It was theorized that performing early defibrillation has no benefit because the heart was not being adequately perfused. This lead to a 2 minutes of CPR prior to shocking in an unwitnessed arrest rule. This is what we, who are AHA compliant, are doing.
CONSENSUS ON SCIENCE:
Two randomized controlled trials (LOE I) (Baker 2008 p424; Jacobs 2005 p39) demonstrated no improvement in ROSC or survival to hospital discharge in patients suffering out-of-hospital VF or pulseless VT who received CPR by EMS personnel for a period of 1.5 to 3 minutes before defibrillation, regardless of EMS response interval being greater or less than 5 minutes. One case series study (LOE IV) (Campbell 2007 p229) also failed to demonstrate improvements in ROSC or survival to hospital discharge with bystander versus no bystander CPR before defibrillation.
One randomized controlled trial (LOE I) (Wik 2003 p1389) and clinical trial (LOE III) (Cobb 1999 p1182) identified overall similar findings however improvements in ROSC, survival to hospital discharge and neurological outcome were observed in patients where the EMS response interval was greater than 4 to 5 minutes.
Evidence from one LOE 1 study (Wik 2003, 1389), one LOE 3 study (Cobb 1999, 1182) and five LOE 5 studies (Berg 2004, 1352; Kolarova 2003, 2022; Menegazzi 1993, 235; Menegazzi 2004, 926; Niemann 1992, 281) support the strategy to delay defibrillation to give BLS first for 1,5 to 8 minutes, in particular when the delay to ambulance arrival exceeds 5 minutes and no BLS is given before ambulance arrival. Evidence from two LOE 1 studies (Baker 2008, 424; Jacobs 2005, 39), one LOE 3 study (Campbell 2007, 229) and nine LOE 5 studies (Berg 2004, 1352; Yakaitis 1980, 157; Menegazzi 2003, 261; Menegazzi 2000, 31; Seaberg 2001, 301; Kolarova 2003, 2022; Niemann 2000, 543; Menegazzi 1993, 235; Rittenberger 2008, 155) do not support this strategy and are neutral. One LOE 5 study (Indik 2009, 179) gave direct evidence for the opposite strategy
Level of evidence - all that LOE stuff you see above is a reference to the grade the mentioned study received by the reviewer.
LOE 1
Randomised Controlled Trials:
These studies prospectively collect data, and randomly allocate the patients to intervention or control groups.
LOE 2
Studies using concurrent controls without true randomisation:
These studies can be:
· experimental - having patients that are allocated to intervention or control groups concurrently, but in a non-random fashion (including pseudo-randomisation: eg. alternate days, day of week etc), or
· observational – including cohort and case control studies
A meta-analysis of these types of studies is also allocated a LOE = 2.
LOE 3
Studies using retrospective controls:
These studies use control patients that have been selected from a previous period in time to the intervention group.
LOE 4
Case series: A single group of people exposed to the intervention (factor under study), but without a control group.
LOE 5So according to the evidence, we may need more evidence. However, there isn't much support to the current guidelines. Once again, do we change this back and confuse more people when we are uncertain if outcomes will improve?
As with other categories of Levels of Evidence, we have used LOE 5 to refer to studies that are not directly related to the specific patient/population. These could be different patients/population, or animal models, and could include high quality studies (including RCTs).
Cardiocerberal Resuscitation or Cardiopulmonary Resuscitation?
Should EMS be doing chest compression only CPR? This is a good question when considering primary cardiac arrest. We know that primary respiratory arrest should involve aggressive airway management.
CONSENSUS ON SCIENCESo there are studies out there, just maybe not enough--once again. There is also research on different compression:ventilation ratios showing promising data. Guess we will find out what really happens in October.
Six fair to good LOE 5 animal studies (Berg 1993, 1907; Berg 1997, 1635; Berg 2001, 2464; Ewy 2007, 2525; Kern 1998, 179; Kern 2002, 645) have shown comparable or better outcomes with continuous chest compression CPR as compared with interrupted compressions for ventilation in nonasphyxial cardiac arrest and in concept support such a change in resuscitation strategy. However animal models do not necessarily mimic the anatomical or arrest features of humans, and for these reasons arguably may be less applicable to human resuscitation. Clinical evidence from three retrospective cohort LOE 3 studies in adults suffering from cardiac arrest (Bobrow 2007, 1158; Kellum 2006, 335; Kellum 2008, 244) showed that provision of chest compressions in the absence of rescue breathing by trained professional (EMS) providers led to an improvement in survival to hospital discharge compared to provision of chest compressions with rescue breathing. However, these studies had methodological shortcomings that limit the ability to determine whether the improvements in survival were attributable to the provision of chest compression-only CPR in the absence of rescue breathing, including the lack of randomization, the implementation of other resuscitation protocol changes that may have affected outcomes, or simply a stronger clinical emphasis on the provision of good CPR. The remainder of clinical studies addressing this issue evaluated the outcome from continuous chest compression versus interposed ventilation CPR by untrained laypersons (bystander CPR),and did not directly address provision of care by trained professionals.

More of the same
There is a lot more evidence out there advocating chest compressions. No pulse checks, just compressions. More and more compressions. Push hard and push fast. Good chest compressions. Are you getting all of this?
Therapeutic hypothermia is gaining more popularity. The evidence is outstanding.
CONSENSUS ON SCIENCE:
Who to cool?
Evidence from one good randomized trial (LOE 1) (HACA, 2002, 549) and a pseudo-randomised trial (LOE 2) (Bernard, 2002,557) demonstrate improvement in neurological outcome after discharge from hospital in patients who had an out-of-hospital VF cardiac arrest, who were still comatose, and who were cooled within minutes to hours after return of spontaneous circulation to 32-34ºC for 12-24 hours. Two studies with historical control groups (LOE 3) showed improvement in neurological outcome after therapeutic hypothermia for comatose survivors of VF cardiac arrest (Belliard, 2007, 252; Castrejon, 2009, 733) One small (n = 30) randomized trial (LOE 1) showed reduced plasma lactate values and oxygen extraction ratios in a group (n =16) of comatose survivors after cardiac arrest with asystole or PEA who were cooled with a cooling cap (Hachimi-Idrissi, 2001, 275). Six studies with historical control groups (LOE 3) showed benefit after therapeutic hypothermia in comatose survivors of OHCA after all rhythm arrests (Bernard, 2007, 146; Oddo, 2006, 1865; Busch, 2006, 1277; Sunde, 2007, 29; Storm, 2008, R78; Don, 2009 3062). One studies with historical controls showed better neurological outcome after VF cardiac arrest but no difference after cardiac arrest from other rhythms (Bro-Jeppesen, 2009, 171). Two non-randomised studies with concurrent controls (Arrich, 2007, 1041; Holzer, 2006, 1792) indicate possible benefit of hypothermia following cardiac arrest from other initial rhythms in- and outof-hospital.
How to cool?
Nine case series (LOE 4) indicate that cooling can be initiated safely with intravenous ice-cold fluids (30 ml/kg of saline 0.9% or Ringer’s lactate) (Kliegel, 2005, 347; Kliegel 2007, 56; Bernard, 2003, 9; Virkkunen, 2004, 299; Kim, 2005, 715 ; Jacobshagen, 2009; Kilgannon, 2008; Spiel, 2009; Larsson, 2010;). Two randomised controlled trials (Kim, 2007, 3064; Kamarainen, 2009, 900), one study with concurrent controls (LOE 2: Hammer, 2009, 570) and three cases series (LOE 3) (Kamarainen,2008, 360;Kamarainen, 2008, 205) indicate that cooling with IV cold saline can be initiated in the pre-hospital phase.
More For Post-Arrest
There is evidence that patients who are resuscitated from primary cardiac arrest should be immediately cathed.
The significance of this new literature cannot be overstated. If further studies confirm these findings, it would strongly argue for enormous changes in prehospital systems of care to recommend that all survivors of primary cardiac arrest should be immediately transported to hospitals that have the capability of performing urgent PCI in conjunction with therapeutic hypothermia. Based on the current literature, it certainly seems advisable that emergency health care practitioners that care for resuscitated victims of primary cardiac arrest should engage in conversations with cardiology consultants and urge them to take an aggressive approach to PCI in these patients.What does this mean for us? Post-arrest 12-lead ECGs for now. In the future, this may mean that we bypass non-PCI facilities with our post-arrest patients. If you think this will last long, you are wrong. Post-arrest patients are high dollar patients. Just think about all of the work-ups done on these patients. Don't think that the non-PCI hospitals won't be rushing to find a way around this. Will this mean more PCI centers? Probably not, because all of the other cardio-intervention seeking patients end up with big medical bills too--but who knows.
Shocking Stuff
So even though AHA came out and said that their initial recommendation for biphasic defibrillators is not backed by any evidence, there may be an actual benefit to having them. There is evidence supporting what I am about to tell you, but it may not make it into the 2010 update. I think it will though. It goes against what we have all learned. Remember "I'm clear, you're clear, we're all clear!"
There is no harm to a rescuer performing chest compressions, when defibrillation is performed using a biphasic monitor.
That's right. It has been said that more electricity passes through your body on one of those scales that checks your BMI than touching a patient when they are getting shocked. It has to be a biphasic defibrillator though.
So that's all so far. Go scan through the worksheets if you'd like. There is a ton of good research available. We can only assume, as of yet, what the final recommendations will be.
At the Florida Emergency Physicians' second annual symposium on critical care in the emergency department, Dr. Amal Mattu (yes, I am mentioning him once again) presented most of these updates. This motivated me to research and share them with you.
12-Lead Differential Diagnosis: Syncope
Adam Thompson, EMT-P | 2:51 PM | Cardiology, ECG/EKG Archive, Education | 0 comments
12-Lead Differential Diagnosis: Syncope
By Adam Thompson, EMT-P
I have decided to use some exerts from my favorite emergency physician/presenter, Dr. Amal Mattu. Dr. Mattu has spoke and written on these topics multiple times.
Bradycardia
This first one is easy, and you wouldn't even need a 12-lead to determine it's malignancy.
What do you notice about the 12-lead above? How about the rate? This is an example of bradycardia. Bradycardia may cause hypo-perfusion, leading to syncope. This would classify them as symptomatic, and they may require treatment.
*It is important to remember that there are many tachycardic arrhythmias that could cause syncope as well.
*It is important to remember that there are many tachycardic arrhythmias that could cause syncope as well.
Acute Myocardial Infarction
An acute myocardial infarction (AMI) is the most common reason we use a 12-lead for diagnostic purposes. An AMI may cause syncope amongst many other signs and symptoms. Syncope would be an atypical (not usual) presentation for an AMI. I am not going to elaborate much on this presentation because it requires much teaching for those who are unfamiliar with STEMIs (ST-Elevated Myocardial Infarction). Please head over to the prehospital 12-lead blog for some great education on STEMIs.
Long QT Syndrome
Long QT Syndrome, or LQTS may lead to arrhythmias that lead to syncope. This happens due to something called an R on T phenomenon. The most common arrhythmia due to LQTS is Torsades de Pointes, however monomorphic ventricular tachycardia is possible. Syncope and/or seizures are common symptoms of the rhythms associated with LQTS.
Torsades de Pointes
From Dr. Amal Mattu:
Prolonged QT-Interval
• Prolonged QT-interval predisposes to torsades de pointes
• One of the key “can’t miss” diagnoses associated with syncope
• Perhaps a more common cause of syncope and sudden death than previously recognized?
Causes of QT-prolongation
• Electrolyte abnormalities (hypokalemia, hypomagnesemia, hypocalcemia)
• Sodium channel blocking medications (many!)
• Includes Type IA medications, anticholinergics, cocaine, many antipsychotics, some antibiotics
• Acute myocardial ischemia (usually associated with inverted T-waves)
• CNS lesions, e.g. intracerebral hemorrhage (often associated with giant inverted T-waves)
• Hypothermia
• Congenital
How long is too long?
• QT-interval will vary based on patient’s heart rate
• Measure QT from beginning of the QRS complex to the end of the T-wave, and average over 3-5 beats
• “Corrected” QT-interval (Bazett formula): QTc = QT/√(RR)
• QTc is considered prolonged when > 450 msec in men and > 460 msec in women and children
• Major risk occurs in patients with QTc > 500 msec
Treatment
• Search for and correct underlying cause (e.g. correct electrolyte abnormalities, discontinue responsible medications, etc.)
• Congenital or idiopathic causes: beta-blocking medications attenuate adrenergic-mediated trigger mechanisms
• Treatment of torsades de pointes: cardioversion/defibrillation, magnesium if relatively stable (e.g. intermittent torsades): 2 grams IV over 2-3 minutes followed by infusion
• Overdrive pacing? Isoproterenol? Atropine? These are listed as possible treatments in acquired (not for congenital) cases, but rarely needed
• Post-conversion treatment with magnesium, not lidocaine/amiodarone/ procainamide! (unlike other forms of ventricular tachycardia); for congenital cases, add beta-blocking medications
Click here or here to learn about Long QT Syndrome
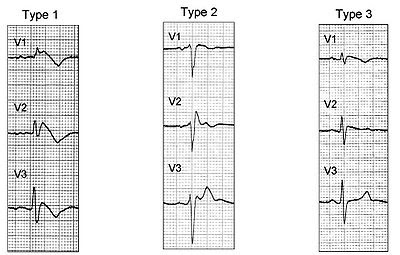
Brugada Syndrome
Brugada syndrome is becoming more and more well known recently. It is associated with specific ECG changes and an increased risk for sudden cardiac arrest. Only known cause of Sudden Unexpected Death Syndrome (SUDS)--according to Wikipedia. The ECG changes associated with Brugada Syndrome are most visible in V1, and V2. Non-STEMI-like ST-elevation that cannot be explained by another pathological cause (ie. LVH, LBBB, BER) may be Brugada Syndrome. These individuals may be otherwise very healthy and/or young.
Some features of the different types of Brugada Syndrome include:
- a RBBB pattern in V1 without terminal S-waves in lead I and V6.
- A saddleback ST-elevation pattern (type 2 below)
- Coved J-point elevation in V1, V2, V3 that gradually slopes down (type 1 below)
From Dr. Amal Mattu:
Brugada Syndrome
More common cause of sudden death than previously recognized
• May be responsible for up to 20% of sudden deaths in individuals without structural heart disease
• Responsible for 4-5% of all sudden deaths
• Incidence varies in different populations (some genetic factors involved)
• Most common in young males (< 50 yo.)
• First onset of symptoms approximately 40 yo.
• Mortality approximately 10% per year if not treated with an internal cardioverter-defibrillator (ICD), regardless of whether or not antiarrhythmics are used
Syndrome characterized by
• ECG abnormalities in leads V1 – V3
• Polymorphic or monomorphic (less common) ventricular tachycardia
• Causes syncope if self-terminating
• Causes sudden death if persists and not terminated by treatment
• Structurally normal heart
• Familial occurrence in approximately half of patients
ECG findings in leads V1 – V3
• Right bundle branch block (RBBB) or incomplete RBBB pattern
• ST-segment elevation — 2 types
• “coved-type” (most common)
• “saddle-type”
• ECG findings can vary with time depending on the autonomic balance, administration of antiarrhythmic and other drugs affecting channel function, body temperature, and other unknown factors
Definitive diagnosis can be made with electrophysiologic testing
• Challenge with an intravenous class I medication (e.g. ajmaline, procainamide, flecainide)
• Will induce increased ST-segment elevation and “coving”
• Programmed electrical stimulation of the heart
• Can induce ventricular tachycardia
Treatment
• Placement of an ICD is the only effective treatment
• Antiarrhythmic drugs (including beta blockers, amiodarone, etc.) ineffective
Click here or here for more on Brugada Syndrome
Hypertrophic Cardiomyopathy
From Dr. Amal Mattu:
Hypertrophic Cardiomyopathy (AKA IHSS, ASH, HOCM, etc.)
• Prevalence — 0.02% – 0.2% of the general population
• Genetic factors involved
• Hypertrophied but nondilated left ventricle
• Thickening is usually asymetric, involving the septum to a greater extent than the free ventricular wall
• Cardiomegaly usually not present on chest x-ray
• Mortality 3.5% per year
• Diagnosis often made only when the patient experiences sudden death
• Usually occurs during exertion \
• Average age at diagnosis is 30 – 40 yo.
• Patients may also experience syncope, angina, palpitations, dyspnea (often associated with exertion)
ECG findings
• Normal in 7% – 15%
• Typical abnormalities
• Deep narrow Q-waves in the inferior and/or lateral leads – I, aVL, V5-6 (simulates MI, but Q-waves are “too narrow” for MI)
• Very specific for this condition
• Q-waves in lateral leads are more common than inferior leads, very commonly misdiagnosed as lateral MI
• Left atrial enlargement
• High left ventricular voltage/left ventricular hypertrophy
• Other less common abnormalities
• Tall R-wave in lead V1 (simulates posterior MI)
• Deep narrow Q-waves in the inferior leads (simulates inferior MI)
• Don’t rely on your cardiologists to make the Dx on ECG! Clinical diagnosis
• Systolic murmur at apex or LLSB
• Murmur increases with valsalva, standing
• Murmur decreases with trendelenburg position, isometric exercise, squatting
• Definitive diagnosis — doppler echocardiography
Treatment
• Beta blockers, calcium channel blockers to improve LV filling and diastolic \function ]
• Amiodarone if ventricular dysrhythmias present
Unrecognized Killers in Emergency Electrocardiography
Amal Mattu, MD 7
Occupational Hazard: Playing the Fool
Rogue Medic | 3:04 AM | Critical Judgment, Heresy, Rogue Medic | 1 comments
Occupational Hazard: Playing the Fool is the title of a must read article by Michael W. Kahn, MD.
It starts out with an important question. Maybe this is a question that might be a good way to screen future health care workers - doctors, nurses, paramedics, et cetera.
“Can you tolerate being bamboozled by your patients from time to time?”[1]
Maybe we should turn the question around.
Is it more important for us to punish some of our misbehaving patients, than to provide appropriate treatment to all of our patients?
Better to punish?
Better to treat?
This is the crux of one dialogue about appropriate pain management.
We deceive ourselves into believing that we can tell who is telling the truth and who is telling a lie. We base this belief on . . . ?
Well, what do we base this on?
Are there any studies that show how to identify the patient telling the truth?
or
Are there any studies that show how to identify the patient is not telling the truth?
Do we demand that our patients have an obvious extremity fracture, just to prove to us that they have pain worthy of treatment?
Why?
If the patient does not have some blatant injury, does that mean that there is no legitimate pain?
Why?
If the patient does not have some blatant injury, does that mean that their pain is not worthy of treatment?
Why?
That looks painful. You may have something for pain.
That doesn't look painful. You get Ultram.*
I think we underemphasize the prevalence of certain normal errors inherent in medical practice. Surgeons are fooled when they open an acutely painful abdomen only to find a normal appendix: in the days before CT scans, it was said that if that didn’t happen once in a while, you weren’t operating often enough. When in doubt, it was safer (and wiser) to operate than to risk a rupture and peritonitis, even if the diagnosis was “wrong.” Here was an error that wasn’t an error, but rather a predictable side effect of balancing known risks with imperfect information.
I suggest that we apply a similar principle to the prescribing of narcotic painkillers and anti-anxiety drugs. Let’s assume that it’s impossible not to be fooled at least some of the time — that when assessing patients’ sincerity, we should expect a certain rate of false positives.[1]
We have no ST scan to identify pain.
Since “first, do no harm” remains a guiding principle of care, let’s remember that the harm of missing a chance to help often greatly exceeds the harm of prescribing under a false pretext. Our system of justice is based on the idea that we should let the guilty go free rather than punish the innocent. Could our prescribing habits benefit from the same philosophy?[1]
Go read the whole article.
Footnotes:
^ 1 Occupational Hazard: Playing the Fool
by Michael W. Kahn, MD
New York Times.
Article
^ * Ultram
Wikipedia entry for tramadol.
Ultram is tramadol, which is just the result of another attempt to come up with a treatment for pain that is effective, but not addictive. The result is a drug that is addictive, but is not effective.
When I hear that a patient is receiving tramadol, it tells me that the doctor believes that the person is a drug seeker, but the doctor is afraid to refuse all pain medicine, so the doctor decides to give something they can document - Ultram.
Ultram = pain relief in documentation only.
.
Prehospital Stroke Care 2
Adam Thompson, EMT-P | 10:24 PM | Clinical Discussion, Education, Neurology | 0 comments
Cerebral Vascular Accident
Clot or Bleed?
By Adam Thompson, EMT-P
The stroke patient is one that is commonly seen and transported by EMS providers. There tends to be a frustration due to the inability to do much for these critically ill patients. Their quality of life subsides right before our eyes. There are two types of stroke as I explained in PART 1. There are treatments available for ischemic strokes that can tremendously benefit the patients if given soon enough. Thrombolytic therapy could be very effective in treating the ischemic stroke patient in the prehospital environment. The only problem is that if this treatment was used on a patient suffering from a hemorrhagic stroke, it could tremendously worsen that patient's condition. There is no way to conclusively differentiate between an ischemic or hemorrhagic stroke in the field without the use of diagnostic equipment. There are, however, many indicators that could clue you in on the probably etiology.
Risk factors for stroke
Most of the risk factors for stroke are the same for both subtypes. However, some are more indicative of a specific type. Knowing these may assist you, along with the presenting signs and symptoms.
More associated with ischemic stroke
- Atrial fibrillation
- History of TIAs
- Increase in Vitamin K
- Carotid artery disease
- High cholesterol
- Diabetes
- Patent Foramen Ovale
More associated with hemorrhagic stroke
- Severe acute hypertension
- Anticoagulant medications
- Smoking
Similar to risk factors, physical findings are not synonymous with a specific subtype, but they are very good indicators. These signs may indicate either type of stroke, I cannot stress that enough.
Signs of Hemorrhagic Stroke
- Airway compromise
- Complete unresponsiveness
- Complete aphasia
- Nausea & vomiting
Signs of Ischemic Stroke
- Expressive aphasia
- Unilateral deficits
- Poor coordination
So it is possible to have a fairly good idea weather the stroke patient you are presented with is suffering from a clot or a bleed, based on a fine assessment. With advancements in technology, this skill, however, may eventually be unneeded. There is solid evidence supporting the efficacy of paramedics and the use of prehospital diagnostic equipment. There are portable brain scanners that are being tested in the field right now. This may sound like something far-fetched or unnecessary, but I believe otherwise. With stroke being the time is tissue condition, why not use equipment that may facilitate treatment that could subsequently improve the quality of life, of our patients. With the ability to conclusively diagnose an ischemic stroke, thrombolysis could be preformed much earlier. There would be an obvious need to provide research and gain evidence to support this process, but with an exponential probability of benefit, there should be a bigger push to get this done. The studies advocating hypothermia in the presence of a CVA all appear encouraging as well. Please read some of the research I have provided below.
A protocol to improve analgesia use in the accident and emergency department
Rogue Medic | 4:25 AM | Critical Judgment, Heresy, Research, Rogue Medic | 2 comments
.jpg)
Last month I pointed out Prehospital use of analgesia for suspected extremity fractures. The study I am covering now looks at a similar group of patients in A&E (Accident & Emergency - the British version of ED - Emergency Department).
We aimed to assess the use of analgesia within our department and identify shortcomings. Having done this we devised a protocol for intervention and assessed whether this was successful. We chose acute skeletal injuries as a well defined group of unequivocally painful injuries that could readily be assessed.[1]
The authors don't even doubt that they have a problem. They already have a plan to fix the problem. They claim that they are looking at a well defined group of unequivocally painful injuries that could readily be assessed. Not all fractures cause moderate to severe pain. Using opioids for minor pain, even if from a fracture, is not good medicine. Even their results do not agree. The doctors in this study do seem to have been equivocal, when it came to the pain of their patients.
Methods
One hundred consecutive referrals to the fracture clinic and 100 orthopaedic admissions were analysed for the following data: (1) patient's sex and age; (2) injury sustained; (3) analgesia given in A&E department: drug used, dosage, route of administration.[1]
Using consecutive referrals is a good way to randomize to avoid selection bias. This is one of the things that Ex-Dr. Andrew Wakefield did that was a reason for eventually retracting his autistic enterocolitis paper, although it was just one of many problems with that paper.
The results of this audit were presented at a staff meeting. An analgesic protocol (figure) was then introduced and circulated through the department to all staff.[1]
Here is the protocol they came up with.
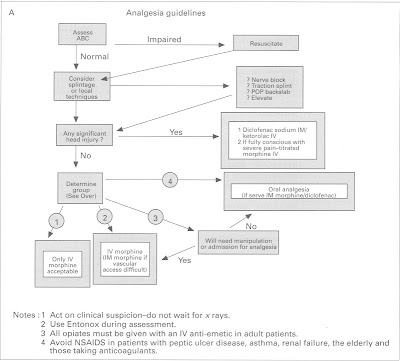
The Notes at the bottom are interesting.
1. Act on clinical suspicion - do not wait for x rays.[1]
This is nice and logical.
An x ray does not tell you anything about the pain the patient is experiencing. Waiting for an x ray does nothing to help the patient. If anything, trying to position a painful injury for x ray, will probably increase the patient's pain and is likely to make it more difficult to obtain a clear x ray.
Waiting for an x ray makes as much sense as delaying treatment of abdominal pain until after the patient is assessed by a surgeon. There is no evidence to support either excuse for delaying pain management.
2. Use Entonox during assessment.[1]
Entonox is a brand of nitrous oxide/oxygen mixture. This can decrease the amount of opioid needed to appropriately manage the patient's pain. Since the goal is pain management, not opioid dose, this is a good thing.
One huge confounder is the complete lack of mention of nitrous oxide anywhere else in the study.
Did all patients receive nitrous oxide?
What about before the study?
If they have been using nitrous oxide and using it aggressively, then their pain management is better than it appears, but why is there no other mention of nitrous oxide. They mention paracetamol, which is the Commonwealth name for acetaminophen, (commonly sold under the brand name of Tylenol), but ignore any mention of nitrous oxide? Nitrous oxide can be an excellent pain medication. Nitrous oxide is not used enough. In this study, we don't know if it was used at all, even though we are presented with a protocol stating Use Entonox during assessment.
3. All opiates must be given with an IV anti-emetic in adult patients.[1]
This could generate a couple of blog posts on its own.
The preferred route of administration for titratable medication is IV (IntraVenous). The use of IM (IntraMuscular) opiate is not a good idea. IM use may be based on a combination of ignorance and being too lazy to start an IV, although the authors suggest that this is a vascular access problem. Maybe.
Why would someone use IV anti-emetic medication in combination with IM pain medication? Given IM, the effect is delayed. Given IM, the ability to titrate is compromised. Given IM, much more medication is required to produce the same effect.
There is rarely a need for anti-emetic medication when treating patients with opioid medications - even with large doses of opioids. It is important to not give the medication as a fast push. Almost all of the adverse effects/side effects are rate/dose related. Either the rate of administration increases the frequency of the side effect, or the total increases the frequency of the side effect, or both. The rate may be most likely to induce side effects during the first dose of a medication, while the total dose may be more likely to produce side effects with the later doses.
An anti-emetic generally produces sedative effects. If we want to sedate the patient, midazolam may be a more appropriate choice.
If nausea is present, I find that morphine or fentanyl will do a great job of decreasing the nausea by decreasing the pain that appears to be causing the nausea.
In one of the Star Wars movies, Yoda explain a problem with fear. However, Yoda does not point out the obvious. Fear also has an origin. Fear is often due to ignorance.
“Fear is the path to the dark side. Fear leads to anger. Anger leads to hate. Hate leads to suffering.”Yoda also stops with suffering, but even suffering is not the worst of it. I would write it this way -
Ignorance is the path to abuse. Ignorance leads to fear. Fear leads to denial. Denial leads to suffering. Suffering leads to self-delusion. Self-delusion leads to complacency.
When we see the suffering we have increased, we delude ourselves about the actual cause of that suffering. We pretend that we are really acting in the best interest of the patient, but aren't we really acting to protect our ignorance?
Self-delusion is what allows us to make up all sorts of excuses for abuse. Once we start deluding ourselves, where do we stop?
Once we start deluding ourselves, do we maintain any reason to examine what we do?
Their pain isn't that bad.
I know a faker when I see one.
Pain builds character.
We don't want to turn them into addicts.
It's a slippery slope.
Once we start treating one patient's pain, we will be invaded by hordes of drug seekers faking hip fractures, tib/fib fractures, humerus fractures, third degree burns, et cetera.
That doesn't hurt.
These drugs are dangerous.
Fentanyl is much too potent.
Respiratory depression will sneak up on the patient and carry the patient off to the morgue before anyone can notice.
It's for your own good.
Man up.
What if . . . ?
The use of these phrases indicates ignorance about the appropriate use of opioid medications.
We should not let the Jenny McCarthys of pain management guide our treatment decisions. We should be educating the ignorant, so that they better understand pain management.
Ignorance is only a problem if it is maintained. We are all ignorant, just on different subjects.
How we deal with our ignorance determines how we treat our patients.
Act on clinical suspicion - do not wait for x rays.[1]
There is a big problem with this study and the previous study I wrote about. They only look at fractures. They do not look at pain. They do not measure pain. They use the fracture as a surrogate for pain. Fractures often are painful.
What does an x ray tell you about the patient's pain?
Not a thing.
The x ray will tell you something about what appears to be causing the pain, but opioids are not a part of the treatment of fractures. Opioids are a part of the treatment of pain.
If the pain is not due to a fracture, but is due to a sprain, or a strain, or a tumor, or an insect bite, or a poisoning, or an embolus, or a burn, or ischemia, or any of the many other causes of pain - should we ignore that pain just because there is no fracture?
No.
We should not ignore pain until after an x ray.
We should not ignore pain until after arrival at the hospital.
We should not ignore pain until after transport.
We should not ignore pain until after immobilization.
We should treat the pain as soon as is appropriate.
If I have a patient with an apparent hip fracture - painful deformity to a leg that appears shortened and externally rotated - I only need to know a little bit of information before initiating treatment. A quick assessment (including circulation, sensation, and movement distal to the injury, vital signs, and pain rating), a list of allergies and medications, and a history. This takes a couple of minutes. I also need IV access. This may take another couple of minutes. Then it is all a matter of give a bit of fentanyl and reassess, repeating every 5 minutes, until the pain is reduced to a level, where it is appropriate to move the patient.
If it takes 10 minutes to manage the pain, that is not a problem.
If it takes half an hour to manage the pain, that is not a problem.
If it takes over an hour to manage the pain, that is not a problem.
These are only problems if we are more worried about our hypothetical next patient than we are worried about our current patient. I am able to provide a significant benefit to this patient, but some people are more interested in some other patient who might benefit more. If we are going to be treating patients, we need to act as if we have the maturity to pay attention to the current patient, not dreaming about other patients with potentially greater life threats.
What if . . . ?
What if we actually provide competent care, rather than worry about the things that are not happening?
What if we really do have other ambulances and mutual aid agreements to deal with more than one call at a time?
What if we have exaggerated the importance of response times beyond what is remotely reasonable?
Over the following one month a further 100 consecutive referrals to fracture clinic and 100 orthopaedic admissions were then assessed using the same criteria.[1]
One nice thing about this is that it makes the percentages of the total easy to work with. 1 = 1%. There were 100 patients in each of the original groups, so it is easy to compare. That is a total of 400 patients, but it would be better with a lot more patients.
Results
FRACTURE CLINIC REFERRALS
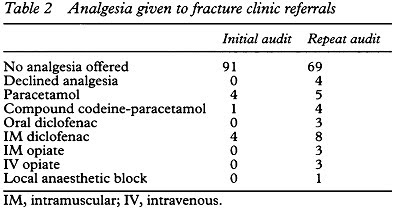
These were divided into four groups: forearm, lower leg/ankle, hand/foot, and others. The numbers of fractures assessed in the initial and repeat audit are shown in table 1. The analgesia given is detailed in table 2. Fracture clinic referrals receiving unsatisfactory analgesia were reduced from 91 % to 69%, a difference of 22% (95% confidence interval 10.9% to 33.1%, P < 0.001).[1]
Let's look at that a little bit differently. If 91% of these patients are receiving unsatisfactory analgesia, then we might conclude that 9% of patients are receiving satisfactory analgesia. After the protocol, this increases to 31%. They describe this as a 22% improvement.
If they were trying to increase sales of a drug, would they be reporting these numbers this way? If a competing drug showed an effect in 3% of patients, and the drug being studied showed an effect in 6% of patients, would the advertisements claim 3% more effective than our competitor? No, they would not. The drug would have doubled the effect. Whether that doubling is relevant depends on a lot of things. The ads would probably claim 100% more effective than our competitor or, the same information expressed for a different effect, 200% as effective as our competitor.
The increase in patients receiving satisfactory analgesia increases from 9% to 31% an increase of 22% of the total number of patients, but an increase of 244% above the original 9%. 22 is almost 2 1/2 times 9.
There are several things to mention about this.
91% unsatisfactory is pretty bad. The authors acknowledged that they were not happy with that. They sought to improve things. The improvement was dramatic.
Imagine if you are back in grade school and you get a score of 9% on a test. We will assume that this was not a grade on a multiple choice test, because unless there were an average of eleven choices for each question, you would be expected to do better by just guessing.
If you have a 9% score on your first test, but get 31% on the next test, are you going to be bragging to your parents? No, you probably are not. It is more likely that you will be offering to get the mail every day for a while. You may be engaging in a bit of triage of mail from the school, or hacking the parents' email to redirect school emails to you.
65% is the minimum score to be considered passing in many places. If you took 31% and doubled it, you still would not receive a passing score. Can you claim that you have learned 244% more between Test 1 and Test 2? That may depend on how little you knew at the time of Test 1.
There is no Limitations section, so I created a sample of what that might include.
What is not reported in this study:
Was there any change in availability of opioids?
Was there any change in supplier of opioids?
Was there any change in requirements for documentation?
Had there been any event before the first part of this study that had staff especially worried about pain management, a worry that might have eased with time?
Were there any incentives offered with the introduction of the new protocol?
Was there anything done to track longer term changes in treatment?
Was there any change in the staffing (different hours, new hires, vacation coverage, et cetera)?
Were there any other changes to the way that the patients were treated?
As you can see, there are many things that are not described as being controlled for in the study. Therefore, we should not presume that any of them have been controlled for. What is the confidence interval based on? Just statistics, or is there some understanding of the potential variables? Since this is an early pain management study, I do not expect that there is the kind of awareness of the relevant variables that the same authors would have today.
How sad is it that a study of pain management published in 1996 is considered early?
What did we base our treatment on before then? Unfortunately, we based our treatment on a lot of misinformation. We still do this, but we are getting better at pointing out the misinformation and correcting those spreading misinformation.
That was the Fracture Clinic. Initially, 91% of patients did not receive any medication for their fractures. None of those patients declined pain medicine.
Since I am writing mostly about opioid medication for pain management, I should mention that in the first part, the number of patients receiving opioids is zero IM and zero IV. 4 patients received paracetamol. A whopping 4 patients received this aggressive treatment. They could have done just as well by going to their medicine cabinet and taking their own over-the-counter medicine.
In the second part, those numbers zoom all the way up to IM opioids = 3 and IV opioids = 3. This is not impressive. This is just something is better than nothing.
For those in America, reading this and saying to yourself, I'm just glad I am in America.
Do you really think that pain management is/was better in America?
If you do think pain management is/was better in America, what do you base that on?
ORTHOPAEDIC ADMISSIONS
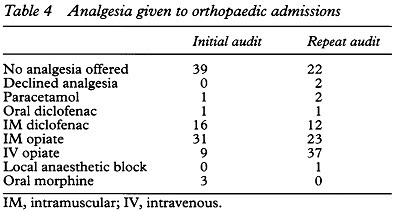
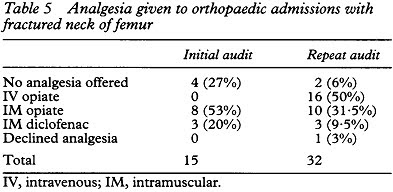
These were also divided into four groups: neck of femur, forearm, lower leg/ankle, and others. The numbers of fractures assessed are given in table 3 and the analgesics used in table 4. Orthopaedic admissions receiving unsatisfactory analgesia were reduced from 39% to 22%, a fall of 17% (95% confidence interval 4.2% to 29.8%, P = 0.009). The number of orthopaedic admissions receiving intravenous opiates increased by 28%, from 9% to 37% (95% confidence interval 16.3% to 39.7%, P < 0.001). The most appreciable improvements in analgesia used were obtained treating patients with fractured neck of femur (table 5).[1]
Orthopaedic admissions receiving unsatisfactory analgesia were reduced from 39% to 22% It is great that we are dealing with numbers that are much higher in this group. Still, this implies that only 61% rated their pain management as acceptable. That improved to 78% after the introduction of their protocol.
Intravenous analgesia is superior to intramuscular analgesia for reasons of speed of onset, reliability of uptake, and the ability to titrate doses to response.4 6 The number of orthopaedic admissions receiving intravenous opiates increased by 28% following the introduction of the protocol.[1]
I have no argument with the reasoning, but they should have already been aware of that before the start of the study. Just as they already should have been aware of this little tidbit - Pain Hurts.
We were particularly successful in improving analgesia for patients with fractured neck of femur. Perhaps the value of intravenous titration of doses is better appreciated in the elderly population who typically suffer this injury.[1]
I would reword that, but I don't think that I am really changing their meaning.
Perhaps the doctors in this study are more comfortable using intravenous titration of doses to better manage the pain in the elderly population who typically suffer this injury (hip fracture).
And by better I mean more safely and with fewer side effects and with faster onset and with a more accurate end point.
This was from the dark ages of pain management, which was only 14 years ago where this study was done. Other places may not have progressed beyond this point, even now. It is good that the authors looked at their practices. I expect that they are much more aggressive today than what is shown in this study.
And for the punchline we have this -
Setting- University teaching hospital.[1]
These are supposed to be doctors with the most education, the most resources, the most experience, et cetera. These are supposed to be the doctors who are educating the doctors of the next generation. Even in an academic medical center, they appear to have been held back by the mythology of pain medicine, but they are changing that mythology.
Discussion
The management of pain in acute trauma is often neglected.1 2 Patients arriving at A&E departments with acute trauma are unlikely to have received sufficient analgesia,3 so responsibility lies with the attending doctor.[1]
Sometimes the best way to encourage the doctors to treat pain appropriately is to authorize EMS to treat pain appropriately. Doctors are capable of both compassion and learning, but sometimes they do seem to need a push. The authors of this study did provide a bit of a push. Did things continue to progress, or did they revert to whatever was the mean at this A&E?
Footnotes:
^ 1 A protocol to improve analgesia use in the accident and emergency department.
Goodacre SW, Roden RK.
J Accid Emerg Med. 1996 May;13(3):177-9.
PMID: 8733653 [PubMed - indexed for MEDLINE]
Free Full Text from PubMed Central
Free Full Text PDF from PubMed Central
.
Subscribe to:
Posts (Atom)