
S.A.L.T. Device
Adam Thompson, EMT-P | 2:21 PM | Airway, Airway Management, Intubation, Product Review | 2 comments

66 year old male CC: Chest pain
Tom B | 1:09 PM | ECG/EKG Archive | 3 comments
Here's another great case submitted by Nick Ciaravella of Grady EMS in Atlanta, GA.
66 year old male presents to EMS with chest pain.
S - Chest Pain
A - None
M - Atenolol, HCTZ
P - HTN
L - meal, 7 hours prior to event
E - Mowing his lawn
O - Started while mowing his lawn
P - Provoked while exerting himself, Palliated initially when he sat down to rest
Q - Sharp
R - Substernal, initially radiating to his jaw, when he rested the pain was only in his chest
S - Initially 10/10, upon ems arrival 4/10, en route 8/10, 9/10, and 10/10 upon arrival at ED
T - No previous episodes
The patient initially presented to EMS with 4/10 pain and vitals as follows, 148/84, pulse 72, 18 respirations, SPO2 96%, Lung sounds clear and equal, BGL 103.
The patient was placed on 3 LPM O2 via NC, given 324 mg Aspirin PO, given 0.4 mg Nitro Tablet Sublingual and then 1 inch of Nitro Paste Transdermal. The Patients pain increased en route to the ED and began to radiate down his left arm en route.
12-lead ECG #1
12-lead ECG #2 (about 15 minutes later)
What do you think?
See also:
Anterior ischemia or posterior STEMI?
26 year old male CC: Chest pain
74 year old male CC: Chest pain
50 year old male CC: Respiratory distress, chest pain
48 year old male CC: Chest discomfort, shortness of breath
Pure (Isolated) Posterior STEMI -- not so rare, but often ignored! - Dr. Smith's ECG Blog
Empathetic vs. Pathetic
Adam Thompson, EMT-P | 8:33 PM | EMS 2.0, EMT, General Discussion, paramedics | 0 comments
PowerPoint Presentation on Strain Patterns!
Tom B | 6:23 PM | Cardiology, Education | 0 comments
This is an awesome PowerPoint presentation from one of my favorite ECG textbooks, 12-Lead ECG - The Art of Interpretation.
You owe it to yourself to purchase this book (and no, they don't pay me to say that).
Make sure you use "full screen" so you can see all of the features of this important presentation. Pay special attention to slides 33-47!
Slide 45 shows a strain pattern from left ventricular hypertrophy (LVH).
Slide 47 shows a split screen with a strain pattern from right ventricular hypertrophy (RVH) on the left and acute infero-posterior STEMI on the right.
This is the book that taught me how to recognize strain patterns! So pay attention because this is one of the most important STEMI mimics!
See also:
Left ventricular hypertrophy - Part I
Left ventricular hypertrophy - Part II
Right ventricular hypertrophy vs. isolated posterior STEMI
Comment on Intravenous morphine at 0.1 mg/kg is not effective for controlling severe acute pain in the majority of patients
Rogue Medic | 6:35 AM | Critical Judgment, Heresy, Rogue Medic | 4 comments
.jpg)
In response to Intravenous morphine at 0.1 mg/kg is not effective for controlling severe acute pain in the majority of patients, there is a comment by medic.
thank you for your post. i'd like to add a few thoughts, and please feel free to comment on them.
Thank you.
1. i have a suspicion that pts who rate their pain 7-8/10 tend to be more honest about their pain than the ones who rate their pain 10/10 (worst pain ever), which perhaps partially explains the study's findings when sorted by initial pain rating.
That may be. Pain is subjective. Out of 119 patients, only 5 rated their pain 7 out of 10, so this is a small fraction that may not indicate anything. If we wish to draw conclusions about patients with 7 out of 10 pain, we need to set up a much larger study and propose our hypotheses before the study is begun.
Even if a report of 7 out of 10 pain is more honest than a report of 10 out of 10 pain, does that make it any less appropriate to treat 10 out of 10 pain aggressively?
2. competence is a huge factor is any setting, not just ems. there are plenty of (supposedly better-trained) docs and nurses who are clearly retarded.
Retarded is not the right word. However many doctors, nurses, and medics just do not get it. Maybe pain management has not been explained to them in the right way.
Many doctors do seem to become much more comfortable using opioids to treat pain after experiencing severe pain themselves.
We never seem to hear about doctors becoming less comfortable using opioids after experiencing severe pain.
This suggests that there is something important that is not understood by the doctors until after experiencing severe pain.
I suspect that studying this might require a huge sample of doctors, just to be able to track the change in prescribing/ordering habits vs. personal experience of severe pain, whether their own pain or the pain of someone they care deeply about.
3. i personally have a high threshold for when i break the narcs open, as i too work in a poor area. that's not to say poor people can't have pain; that's just taking into account other factors such as a seemingly higher rate of drug use/abuse.
It isn't our pain threshold that matters, but the patients' pain threshold.
Opioids are not the appropriate treatment for all pain, but it is appropriate to treat severe pain aggressively with opioids when nothing else works (such as when nothing else is available). Nitrous oxide is something that can be safely used that might significantly decrease the amount of morphine needed to manage severe pain.
4. once i make the decision to use narcs, i am not stingy with them as experience shows that prehospital morphine doses are clearly inadequate. the more important issue here is a training crews for a heightened awareness of the potential for respiratory depression and allergic reactions (just had one last week).
And what did you need to do for the allergic reaction? Diphenhydramine?
Just because something happened last week, does not mean that it is common. We need to be aware of the potential for allergic reactions with all of our medications.
One of the many advantages of fentanyl, over morphine, is that fentanyl is much less likely to produce an allergic reaction.
Recognizing and dealing with respiratory depression should not require anything more than competently monitoring the patient.
Many, but not all, patients will experience respiratory depression with appropriate pain management, because pain tends to stimulate a sympathetic response. Having respirations decrease to normal is a good thing, even though this is respiratory depression.
If the patient shows signs of inadequate oxygenation/ventillation due to respiratory depression, then all that needs to be done is to get the patient to talk. Find a subject that the patient is interested in, people love to talk about themselves, and get them to keep talking. Or just keep asking questions that are not answered with a nod, or shake, of the head. Ask orientation questions. Even just telling the patient to take a deep breath every so often will work.
A talking patient is a breathing patient.
5. it's a big training issue to get crews to recognize those pts who are in pain and those who are trying to score narcs. this is where experience counts and it's difficult to teach. that being said, it's risky to presume that people are trying to score narcs.
We should not presume that people are trying to manipulate us to give them drugs inappropriately. We should be aggressively looking for indications that the patient has legitimate pain.
If I need to give out morphine and fentanyl to a bunch of junkies in order to avoid missing some patients with legitimate pain, then I will be the candy man.
Let me put this in perspective.
If I need to give out albuterol nebulizer treatments to a bunch of people who do not need nebulizer treatments in order to avoid missing some patients with legitimate asthma/emphysema/bronchitis, then I will be the nebulizer man.
If I need to give out IV dextrose to a bunch of people who do not need to receive dextrose through an IV in order to avoid missing some patients with legitimate hypoglycemia and an inability to take glucose by mouth, then I will be the dextrose infusion man.
If I need to take some people with minor injuries to a trauma center in order to avoid missing some critical trauma patients, then I will be the minor trauma man.
I am not encouraging over-treatment, for the sake of over-treatment. We do need to be much better at assessment, rather than treating mechanism. How much training do we have at recognizing drug seekers, who are not seeking drugs for legitimate pain? If we are trained at this in paramedic school, or on the job, what are the qualifications of the person providing this training? What research has been done to demonstrate the accuracy of the methods of differentiating between legitimate drug seekers and illegitimate drug seekers?
The best way to make someone a drug seeker may be to under-treat their pain.
Our concern needs to be much less on being police and much more on being paramedics.
.
62 year old male CC: Chest pain
Tom B | 4:46 PM | Cardiology, ECG/EKG Archive, Education | 0 comments
62 year old male presents to the emergency department complaining of chest discomfort.
** Update 05/19/2010 **
After oxygen and nitroglycerin the patient reports a significant decrease in pain.
An additional 12-lead ECG is captured.
There is now slightly less ST-elevation in leads V3 and V4.
Remember that a secondary ST-segment abnormality (as opposed to a primary ST-segment abnormality) should not "improve" with oxygen and nitroglycerin!
In other words, if this ST-elevation was caused just by the LBBB, it shouldn't be "getting better". Changing ST-segments suggest the dynamic supply vs. demand characteristics of ACS!
Now, let's go back to the initial 12-lead ECG. Is the ST-elevation in the anterior leads cause for concern?
Go back and read Identifying AMI in the presence of left bundle branch block (or paced rhythm). Remember, discordant ST-elevation = or > 5 mm is the least specific of Sgarbossa's criteria! That's why we use the modified rule that I learned from Dr. Stephen Smith of Dr. Smith's ECG Blog.
That criterion states that discordant ST-elevation should not be more than 0.2 (or 20%) the depth of the S-wave in the setting of left bundle branch block (ST/S ratio).
Using that criterion, how does this ECG measure up? Let's take a look.
Ladies and gentlemen, we have a winner!
The patient was ultimately cathed and angiography revealed 100% occlusion of the LAD.
Final thought:
Does it get any more difficult that that? If Dr. Smith's decision rule works this great, shouldn't we be shouting it from the rooftops?
See also:
Discordant ST-elevation in LBBB or paced rhythm
Identifying AMI in the presence of LBBB
Sgarbossa's criteria - new graph
"New" LBBB - What's the big deal?
New left bundle branch block is a poor indicator of coronary occlusion - Dr. Smith's ECG Blog
STEMI best seen in PVC (Dr. Smith's ECG Blog)
Prehospital use of analgesia for suspected extremity fractures
Rogue Medic | 1:47 AM | Heresy, Research, Rogue Medic | 2 comments
.jpg)
This is an older study that puts the prehospital pain management problem into a bit of perspective. While prehospital pain management has improved a lot in some places, other places may still be handling pain as described in this study. This is only ten years old. Attitudes are not changed so easily.
The authors looked at what is probably the least controversial type of pain management. If you were to ask medical directors what they feel most comfortable having paramedics use opioids to treat, the only other choice is likelty to be pain due to burns. Chest pain became a bit controversial after the CRUSADE study, but I will get to that in another post.
Over the last decade, pain and its management have received considerable attention. Most notably members of the medical profession in general and specifically emergency medical professionals undertreat pain to a considerable extent.3[1]
While I would love to be able to defend everyone from this charge euphemistically referred to as undertreatment, the reality is that a decade later, the problem has not changed that much.
This was an observational study involving a retrospective review of all emergency medical services (EMS) runs for suspected extremity fractures[1]
During the study period, all EMS run reports were evaluated by the fire department’s quality assurance coordinator. Only reports documenting the paramedic’s impression that the patient had sustained a fracture, or suspected fracture, of any extremity were included in the database.[1]
There is no mention of any requirement to document any kind of measurement of pain. This seems to be the most significant problem with pain management in the system studied. How do we assess the quality of pain management if we do not assess pain?
The whole structure of this study revolves around the apparent inability to assess pain. There are a bunch of conclusions drawn. Here is what may be the most important omission of the study.
If we do not assess something, how do we treat it appropriately?
If a medical director does not make it clear that pain assessment and management are taken seriously, then is there much reason to expect the paramedics to be more aggressive than the medical director?
We need to provoke medical directors, emergency physicians, emergency nurses, EMTs, and paramedics to take pain seriously.
It's not my pain.
Akron Fire EMS employs a two-tiered transport system whereby nonurgent patients who may be safely transported in a private vehicle are deemed code 1, allowing the med unit to be put back into service. Nonurgent patients who require ambulance transport to the hospital become code 2 and their care and transport to the hospital are transferred to a private ambulance. A patient requiring immediate transport, medication, or procedures rendered by a paramedic is transported directly to the hospital as a code 3.[1]
The two-tiered structure of this EMS system may unwittingly serve to negatively affect the administration of pain medication in several ways. Administering pain medication to a code 2 patient, for whom transport to the emergency department would be transferred to a private ambulance, would automatically change the run to a code 3. Upgrade to a code 3 would necessitate transport directly to the emergency department by the treating paramedic squad, extending the time required to complete the run.[1]
Another question is whether code 3 means a lights and sirens transport to the ED. What extremity fractures, other than those cutting off circulation, require such rapid and rough transport? Even fractures cutting off circulation are unlikely to benefit from the slight difference in transport time that lights and sirens would provide. Slightly faster, but much rougher and much more painful in spite of the pain medicine! Why?
How did this service do at using pain medicine to manage suspected extremity fractures, which are expected to have a high correlation with severe pain?
A total of 18 patients (1.8%) received treatment for pain; nitrous oxide was administered to 16 patients (1.6%), and morphine sulfate to two patients (0.2%).[1]
We know that 16 patients (out of a thousand patients with suspected extremity fractures) received nitrous oxide and 2 patients (out of a thousand patients with suspected extremity fractures) received morphine.
We do not know if they were being treated for pain, since there is no indication of any assessment of pain. We expect that the patients with suspected extremity fractures would have a lot of pain. If you have ever had a painful extremity fracture, you might expect all extremity fractures to be painful. You might also desire that many, most, or even all of these suspected extremity fractures be treated with pain medicine. The authors do not provide anything to support this conclusion.
Let's look at the injuries documented.

All of them seem as if they would be painful fractures. Still, we do not know anything about the pain of these patients.
What else was done that might have acted as pain management?
Supportive medical treatment provided included air splints (25% of patients); full immobilization (19%); ice packs (17%); bandages/dressings (16%); and intravenous lines (9.4%).[1]
Air splints may help to relieve pain by positioning the extremity in a less painful, assuming there is any pain, position. Splinting may temporarily increase pain during application.
Full immobilization is unlikely to provide any pain relief. Full immobilization on a solid long spine board is expected to increase pain.[2]
Ice packs can increase pain, decrease pain, or both.
Bandages/dressings might provide some stabilization, or pressure, that decreases the sensation of pain.
Intravenous lines are often painful. If I only suspect an extremity fracture, I would not have any other justification to be starting an IV, except to have a route to deliver IV pain medication. 2 patients received IV pain medication. 94 patients received IV lines. 2/94?
Did one medic start a line, while the other medic contacted medical command. Since The care of each patient is discussed with an online medical control emergency physician in a local emergency department, the superfluous medic may use that time to get online medical control emergency physician contact out of the way, so that the medic can do something useful, such as assessing or treating the patient.
Did the online medical control emergency physician give this counter-order to the medics? Do not follow your standing orders for pain management. Do not give any pain medicine.
Were the medics, or was one of the medics, hesitant to provide any pain medicine without first contacting the online medical control emergency physician?
Are the medics routinely yelled at by emergency physicians if they administer pain medicine without requesting permission first, even though protocols allow them to give pain medicine without asking for permission?
Do administrators receive complaints from emergency physicians when medics follow standing orders for pain medicine?
The number of patients receiving morphine is so small, that I want to know what was so bizarre about these patients that these Just say No! paramedics gave morphine.
Was the morphine given on standing orders?
Was the morphine even given intentionally?
Since giving morphine for suspected extremity fractures is such a freak occurrence in this system, is there any evidence to suggest that these were not 2 medication errors?
Is the occurrence of morphine administration any less rare than the system's occurrence of medication errors?
The use of morphine is so breathtakingly out of the ordinary in this system, that I do not see any reason to conclude that there is any connection between morphine and suspected extremity fracture. Were any other medications, aside from nitrous oxide, given to any of these patients? Were any of those medications given more frequently than morphine? 2/1,000 suspected extremity fractures.
The EMS pain control policy included standing orders for administration of either morphine sulfate (adult dose: 2–5 mg intravenous push [IVP], may repeat x 1; pediatric dose: 0.1 mg/kg) or nitrous oxide (50%), self-administered. The care of each patient is discussed with an online medical control emergency physician in a local emergency department. By protocol, analgesic therapy is contraindicated in patients with the following conditions: altered level of consciousness; alcohol or drug use; allergies to morphine or nitrous oxide; hypotension; head injury; chest injury with suspected pneumothorax; abdominal pain with possible bowel obstruction; symptomatic asthma or chronic obstructive pulmonary disease (COPD); or respiratory distress.[1]
Even with standing orders, patient care must be discussed with a doctor. In that case, are they really standing orders? There are a lot of contraindications. I almost expect to see suspected extremity fracture listed as a contraindication for morphine. How much different would the results be, if that were the case?
2/1,000 vs 0/1,000.
Is this number, 2/1,000, even close to being statistically significant?
We don't know how many of the 1,000 patients actually had pain that would be appropriate to treat with morphine.
This study examined the use of analgesia in 1,000 prehospital patients with suspected fractures of the extremities who were treated by paramedics. Of the 1,000 patients, only a very few (1.8%) received any pain medication, although morphine sulfate and nitrous oxide were available to the paramedics by both standing order and direct physician order through online medical control.[1]
I think it is misleading to suggest that there was any encouragement by medical command to treat patients with morphine. However, I have no way of knowing if one, or both, of the patients treated with morphine only received morphine because the doctor ordered it.
My experience with online medical command has been one of repeated refusal to give orders for for pain medicine for patients with pain - pain that I would be authorized to treat on standing orders under my current protocols.
What is the difference?
The patients treated with morphine do not suffer as much. The medical command physician does not get to exercise a medical whim to deny pain medicine purely due to the physician's lack of understanding of pain management.
The mean time spent on the scene for all patients in the study was 23 ±3.4 minutes. Scene times were significantly longer for patients who received pain medication (n = 18) 32.8 ±17.4 minutes, than for those who did not, 22.8 ±10.4 minutes (95% CI 5.22 to 14.58). Transport times to the area hospitals average 7 minutes in this system, with the three main receiving hospitals located in the same geographic area. [1]
Unless a patient is unstable (or at risk of injury if not moved), there is no good reason to transport the patient until after the pain is managed. It does not matter if this means an extra 5 minutes on scene or an extra hour on scene. More aggressive dosing (morphine 0.1 mg/kg followed by 0.05 mg/kg every 5 minutes until significant relief) and more appropriate medication (fentanyl at appropriate doses) will result in less time on scene. We should not be manipulating painful injuries until after the pain is managed, unless there is some good reason. That is rare.
When I call for orders for more pain medicine, because the standing orders have not been appropriate in managing pain, medical command often wants to know how far I am from the hospital. My response is, That depends on how quickly I get orders for appropriate pain management, because the patient is not being moved until the pain is managed. Why isn't that obvious to everyone?
Why increase the patient's pain to move the patient to bring the patient to the pain medicine in the hospital, when the patient can be treated just as safely, if not more safely, before being moved?
Second, the administration of nitrous oxide requires that in addition to directly transporting the patient, the paramedics must also exchange the used nitrous tank for a new one. In Akron, the only tank exchange site was located in a remote part of the city, necessitating extended duties and travel time for one of the paramedics. Upon completion of this study, replacement nitrous tanks were placed in each of the 12 fire houses to facilitate more convenient restocking.[1]
It is good to see that they are trying to make things better for patients by eliminating the excuses used by paramedics, when medics rationalize avoiding treating patients appropriately.
Managing pain in the prehospital setting may require a multifaceted approach. Pain experienced by the patient must be evaluated in an objective manner, and once assessed, managed appropriately. Prehospital care providers should be encouraged to appreciate their patients’ pain and given the tools and affirmation needed to provide the most appropriate care.[1]
Yes.
CONCLUSION
Prehospital care providers and their medical control supervisors have room to improve the quality of pain control in the prehospital setting. In this review of the use of analgesia for patients with suspected fractures of the extremities, pain medication was rarely used. Improvements in both the recognition and assessment of pain and in treating the pain in the prehospital setting are slow to be implemented. Education, pain control evaluation, protocol development, and quality assurance and audit systems are all measures that can be used to improve the quality of pain management in the prehospital setting.[1]
All good points, but the most important point is not in there.
Pain management is about treating pain, not treating specific medical conditions.
If you look at all of the contraindications to the use of pain management in this study, there appears to be a strong bias against treating many painful conditions that are not medical contraindications. These appear to be just demonstrations of discomfort with pain management and ignorance of appropriate pain management. As critical as I am of this study, at least the authors are working to improve the way their system manages pain. Most systems seem to deny that there is a problem.
We need to educate prehospital providers to be much more aggressive with pain management.
We spend so much time worrying about paramedics being too aggressive with pain management, but nobody seems to be able to come up with any evidence to support this paranoid fantasy.
We need to provoke medical directors, emergency physicians, emergency nurses, EMTs, and paramedics to take pain seriously.
Footnotes:
^ 1 Prehospital use of analgesia for suspected extremity fractures.
White LJ, Cooper JD, Chambers RM, Gradisek RE.
Prehosp Emerg Care. 2000 Jul-Sep;4(3):205-8.
PMID: 10895913 [PubMed - indexed for MEDLINE]
^ 2 Unnecessary out-of-hospital use of full spinal immobilization.
McHugh TP, Taylor JP.
Acad Emerg Med. 1998 Mar;5(3):278-80. No abstract available.
PMID: 9523943 [PubMed - indexed for MEDLINE]
Standard backboard immobilization is not harmless and can cause significant pain, especially at the occipital prominence and lumbosacral areas. Within 10 minutes of being placed in FSI, Hamilton and Pons12 showed that volunteers developed moderate to severe pain. After 30 minutes in FSI, Chan et al.13 found 100% of volunteers complained of pain, with 55% of the group grading their pain as moderate to severe in quality. Interestingly, 29% of the subjects developed new symptoms over the course of the next 2 days. Chen et al. concluded that “the standard process of immobilization may complicate the evaluation of the trauma patient by generating additional symptoms . . . leading to unnecessary laboratory tests and radiographic studies, time of immobilization, and ultimately, health care costs.” In addition to pain, FSI can cause changes in pulmonary function. can cause pressure ulcers of the buttocks, scalp, or neck, and can increase the risk of aspiration after vomiting.13,14 Because standard FSI can compromise maternal and fetal circulation, it is relatively contraindicated in gravid women.^ 12 The efficacy and comfort of full-body vacuum splints for cervical-spine immobilization.
Hamilton RS, Pons PT.
J Emerg Med. 1996 Sep-Oct;14(5):553-9.
PMID: 8933314 [PubMed - indexed for MEDLINE]
^ 13 The effect of spinal immobilization on healthy volunteers.
Chan D, Goldberg R, Tascone A, Harmon S, Chan L.
Ann Emerg Med. 1994 Jan;23(1):48-51.
PMID: 8273958 [PubMed - indexed for MEDLINE]
^ 14 A review of spinal immobilization techniques.
De Lorenzo RA.
J Emerg Med. 1996 Sep-Oct;14(5):603-13. Review.
PMID: 8933323 [PubMed - indexed for MEDLINE]
.
EMS Week 2010
Adam Thompson, EMT-P | 9:56 PM | General Discussion | 2 comments
67 y/o male CC: Syncope
Adam Thompson, EMT-P | 1:10 PM | Case Reviews, ECG/EKG Archive | 12 comments
His Vital Signs
HR correlates with monitor, pulse not palpable at radial.
Initial BP 78/60
AAOx3, normal mental status, just wants to make a bowel movement.
Skin - Pale, more pronounced and white from the waste down. Skin was relatively dry.
First Possibility: Right-sided infarct with hemodynamic compromise leading to a syncopal episode. The syncope caused a secondary head injury which cerebrally herniated during transport. I would like to note that this is highly unlikely. Also, the patient did not improve with fluids, which would have happened with a traditional RV infarct.Second Possibility: It is much more likely that the patient had an atypical hemorrhagic stroke that presented with the first symptom of syncope. The changes on the 12-lead ECG could just be concurrent with cerebral ischemia. This is not completely understood, but theories involving nerve endings in the myocardium are abundant. The patient's ICP would have increased during transport with the final result being cardiac arrest.Third Possibility: Abdominal aortic aneurism with severe secondary cerebral ischemia due to hemodynamic instability. I'm not fond of this idea even though the AAA fit the picture in the beginning, it does not explain the decorticate posturing.
Improving AHA
Adam Thompson, EMT-P | 6:02 PM | Education, General Discussion | 4 comments
MedicCast - EMS and Health Care Workplace Violence on Federal Radar
Rogue Medic | 1:05 AM | Critical Judgment, Heresy, Rogue Medic | 0 comments
.jpg)
Jamie Davis at the MedicCast writes - EMS and Health Care Workplace Violence on Federal Radar. He also refers to a MedicCast podcast that has not yet been posted, but will be worth listening to when it is posted.
I completely agree with what he writes.
As with people who are not convicted of crimes, because of extenuating circumstance (such as a low blood sugar), the lack of conviction does not mean that the violence did not happen. The lack of a criminal conviction does not mean that nobody was hurt or killed. The lack of a criminal conviction does not even mean that an arrest was inappropriate.
We are covering up violence by not reporting violence.
We are encouraging violence by not reporting violence.
We are pretending that violence that did not result in hospitalization did not happen. Then we are surprised when there is violence that results in hospitalization. When we provide excuses, we encourage excesses.
This is also a problem in the hospital. Nurses are discouraged from reporting violence and from pressing charges. We need to do a much better job of reporting violence.
I continually criticize Zero Tolerance Laws, because the idea that everything in the same category should be treated with at least some punishment completely ignores that the category will include things that do not deserve punishment. On the other hand, I support Zero Tolerance reporting of violence.

Translated from French, the painting states, This is not a pipe. This is true, since it is a picture of a pipe. Rene Magritte's The Treachery Of Images is often used to make this point.
If a picture of something were the same as the object portrayed, I would take this picture of gold bars from Fort Knox to someone who could pay me for the gold. This would quickly destabilize civilization, which would not be a good thing. As it turns out, the image is from an article about fake gold bars in Fort Knox. How would we be able to tell the difference between a picture of the real thing and a picture of a fake? Since a fake is creating an image of the real thing, would it matter?

How is this relevant?
One of the problems with Zero Tolerance Laws is that they do not make this distinction between reality and appearance.
Zero Tolerance Laws mandate punishment for a politically incorrect appearance.
Zero Tolerance Laws discourage judgment - Sentence first, verdict afterward.
Zero Tolerance Laws are designed to prevent us from thinking, because What if somebody makes a bad decision?
Zero Tolerance Laws are excellent examples of extremely bad decisions.
Zero Tolerance reporting helps to make us aware of the problem and helps to do something about the problem.
Zero Tolerance reporting of violence is a way to learn just how bad a problem is.
Zero Tolerance reporting of violence is a way to prevent violence from being ignored.
Assaults on medical personnel are a real problem.
Assaults on medical personnel are not imaginary.
We need to start acting as if the lack of reporting of violence means that violence is not real.
Today, Magritte might paint a picture of an assault on a doctor/nurse/EMT and write This is not a reported assault. Imagine if we were to do something completely crazy - imagine if we were to face reality.
Go read what Jamie wrote. He is the one providing the details about workplace violence and medical personnel.
.
26 year old male CC: Chest pain
Tom B | 6:56 AM | ECG/EKG Archive | 2 comments
Prehospital 12-Lead ECG Efficiency
Adam Thompson, EMT-P | 10:38 PM | Cardiology, Education, EMS 2.0, General Discussion, Research | 14 comments

Recently I have taken part in a very interesting discussion on the NAEMSP dialog page. This discussion is based on the paper Early Cardiac Cath Lab Activation by Paramedics for Patients with STEMI on Prehospital 12 Lead ECGs. Tom B from The Prehospital 12-Lead blog, and contributing author to Paramedicine 101 is one of the active participants in the discussion.
THE POSITIVE PREDICTIVE VALUE OF PARAMEDIC VERSUS EMERGENCY PHYSICIAN INTERPRETATION OF THE PREHOSPITAL 12-LEAD ELECTROCARDIOGRAM
Background. Obtaining a prehospital 12-lead ECG may improve triage and expedite care of patients with acute myocardial infarction (AMI). Whether the ECG should undergo physician review prior to activation of a percutaneous intervention (PCI) team is unclear. Objective. To document the positive predictive value (PPV) of the prehospital 12- lead ECG when interpreted by paramedics versus emergency physicians. Methods. This was a prospective, observational study. In November 2003, our local health care and emergency medical services (EMS) systems implemented a prehospital “cardiac alert” program in which patients suspected of having ST-elevation myocardial infarction (STEMI) based on the prehospital 12-lead ECG were diverted away from receiving facilities without emergent PCI capability and the PCI team was mobilized. For the first year, a cardiac alert was activated by paramedics (Phase I). After the first year, the ECG was transmitted to the ED, with the emergency physician (EP) responsible for activation (Phase II). The PPV for cardiac alerts in Phases I and II were compared by using three different “gold standards”: cardiologist interpretation of the prehospital 12-lead ECG, disposition to emergent PCI, and coronary lesions on angiography or arrest prior to emergent PCI. Results. A total of 110 patients were enrolled (54 in Phase I, 56 in Phase II). Cardiologist confirmation of a STEMI on the prehospital 12-leadEKGwas 42/54 (78%) in Phase I and 54/56 (96%) in Phase II. Disposition to emergent PCI occurred in 38/54 (70%) Phase I patients and 51/56 (91%) Phase II patients. Lesions at catheterization or arrest prior to emergent PCI were observed in 41/54 (69%) of Phase I patients and 50/56 (89%) of Phase II patients. All of these comparisons achieved statistical significance (p less than 0.01) Conclusions. Transmission to the ED for EP interpretation improves the PPV of the prehospital 12-lead ECG for triage and therapeutic decision-making.-PREHOSPITAL EMERGENCY CARE 2007;11:399–402
Intravenous morphine at 0.1 mg/kg is not effective for controlling severe acute pain in the majority of patients
Rogue Medic | 2:32 PM | Critical Judgment, Heresy, Research, Rogue Medic | 2 comments
.jpg)
The EMS Garage also covers pain management on the 5/08/10 podcast. Pain Management: EMS Garage Episode 85. Go listen to that, as well. Chris Montera, Dr. Keith Wesley, Will Dunn, Kyle David Bates, Kelly Grayson, and I discussed several aspects of prehospital pain management.
I have been meaning to cover the research on prehospital pain management for a long time. I did write about one excellent study of fentanyl.[1] Currently, the big obstacle is that there is now so much research to cover. Back in the 1990s, when I would try to persuade doctors that prehospital pain management was safe, there was very little to show to support that statement. A common medical command order was for 0 mg morphine, but we could repeat that as often as we liked. Some times we would get orders for 2 mg morphine and sometimes have the possibility of repeating that dose one time.
From the title of this, you can see that the authors take a dim view of that kind of dosing. Intravenous morphine at 0.1 mg/kg is not effective for controlling severe acute pain in the majority of patients.[2] This study was just on adults, so we should consider the size of an adult. I consider ballpark figures for a small adult to be 50 kg (110 pounds), a medium sized adult to be about 80 kg (176 pounds), and a large adult to be about 110 kg (231 pounds), although there does not seem to be any shortage of people significantly larger than that.
Using these very rough estimates, 0.1 mg/kg would be 5 mg morphine for a small adult with severe pain. The title of the article states that this dose would be inadequate for most patients with severe pain. If the common doses of morphine that used to be given were 0 mg, 2 mg, and 4 mg, were we doing anything more than relying on the placebo effect for the majority of pain relief?
If 5 mg is inadequate for a small patient with severe pain, 8 mg is inadequate for a medium patient, 11 mg is inadequate for a large patient, and there are plenty of much larger patients, what good was a typical dose of 2 mg morphine, assuming that the doctor would be generous enough to even give orders for this dose? Another reason for putting off writing about this has been my attempt to avoid making this just a rant about neglect of patients with severe pain.
Let's assume that you are not a misanthrope. You are not the kind of person to hurt strangers, just because you can get away with it. You might even occasionally apply the Golden Rule of Do to others as you want them to do to you. What would you want done to you?
0 mg morphine? This can be roughly translated to non-medical terminology as, What are you crying about? I am the one who has to listen to your crying!
2 mg morphine? Even for the small adult, this does not come close to the 0.1 mg/kg that the authors state is inadequate.
2 mg morphine with a repeat dose of 2 mg morphine? At least we are moving away from a complete placebo dose in the small patient, but in the medium sized patient, this is not much different from the single dose of 2 mg for the small patient. For the large patient, this is still just a placebo. For the extra-large patient this is just a very bad joke.
After all of that, what does the actual study state?
A standard means of taking into account the heterogeneity of analgesic response in treatment is titration of dosage, with small increases of dose over short periods of time. Some emergency medicine texts recommend a range of doses (eg, 0.05 to 0.15 mg/kg)6; others provide a single dose (eg, 10 mg)7 or a single weight-based dose (0.1 mg/kg)8 with the proviso that the dose should be titrated to desired analgesic effect. There is little evidence about whether these recommendations are routinely followed in ED care.
Although titration is a goal for optimal management of acute pain, a first step is to assess the recommended starting dose. Given the various recommendations for intravenous morphine, ranging from 0.05 mg/kg to 10mg, we chose to assess the analgesic response to the recommended weight-based dose of 0.1 mg/kg. The purpose of this investigation was to quantify the proportion of patients in acute pain who had less than a 50% reduction in pain intensity 30 minutes after intravenous administration of 0.1 mg/kg of morphine.[1]
Arguments can be made that this endpoint is as valid as reduction of pain to less than 3 out of 10. Farther down, I will compare the results if 3 out of 10 had been used.
patients were eligible if they were between 21 and 65 years of age, spoke English or Spanish, or had acute pain with onset within the past 7 days. Exclusion criteria included previous use of methadone, use of other opioids or tramadol within the past 7 days, previous adverse reaction to morphine, chronic pain syndrome, altered mental status, pregnancy, use of monoamine oxidase inhibitors in the past 30 days, systolic blood pressure less than 100 mmHg, or inability to provide informed consent.[1]
All reasonable exclusions.
Patients were asked by the research associates to rate their pain intensity at baseline and 30 minutes post baseline. Peak analgesia from intravenous morphine is achieved within 5 minutes of administration in most patients.9,10 Clinically, 30 minutes seemed to be a reasonable time within which adequate analgesia should be achieved in patients with severe pain. Further, it is unlikely that an analgesic effect would be missed with this interval because the elimination half-life of morphine is 2 to 4 hours.9,10[1]
I confess. I only checked the abstracts for footnote 9[3] and footnote 10[4] cited for morphine reaching peak effect within 5 minutes. I do not feel that 5 minutes is accurate for peak effect. For peak serum levels, 5 minutes may be correct. When acute pain patients start discussing their serum morphine levels with me, then I will wonder about this, but not before then. I will address the onset of effect of morphine and the peak effect in covering other acute pain research that more directly addresses this.
I feel that an assessment of pain at 30 minutes will not miss a significant amount of the pain relief that morphine will provide.
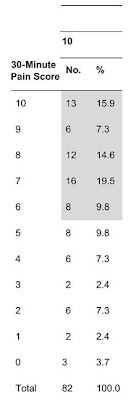
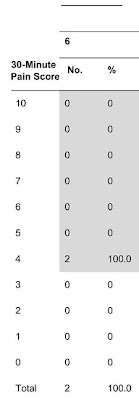
On the side, I have provided parts of the chart from the study that shows the change in pain levels at 30 minutes. this is the caption - Figure.
Distribution of 30-minute pain score by baseline pain score.*
*Shaded area indicates number and percentage of patients whose pain scores decreased <50%.[1]
In other words, if a patient's rating of their pain started at 10 out of 10, the shaded area extends down to the top of 5 out of 10. If a patient's rating of their pain started at 8 out of 10, the shaded area extends down to the top of 4 out of 10. You can see how many patients remained in the less than 50% relief by the shading.

Pain is generally rated on an 11 point scale from 0 being no pain. Some people like to start at one, feeling it is more important to have the scale only have ten points, but end at ten. So 1 is nothing for them. I feel much more comfortable explaining to patients that nothing means nothing. Actually, I find that I do not have to explain the concept of zero. For somebody experiencing severe pain, I expect that zero is their desired level of pain. 10 is the worst pain imaginable. On the podcast, Dr. Wesley has a very creative way of describing the worst pain imaginable.
For the patients starting with the pain level of 10 out of 10, 68.1% did not have relief of at least 50%. That number really does not tell us a lot, but it is less than one third, so that means a lot of patients with very little relief. We are not describing complete relief of pain, but only a reduction of 50%. Less than 1/3 having a 50% reduction in pain level is pathetic.
15.9% had no relief at all. None.

15.8% had a decrease in pain to 3 out of 10 or less. The difference is just due to rounding. Both percentages represent 13 out of 82 patients. I added up the fractions, so that the numbers on the chart match my numbers. For patients with an initial pain level of 10 out of 10, a decrease of 50% is expected to be much more likely, because the target also includes patients with a decrease in pain to 4 out of 10 and patients with a decrease in pain to 5 out of 10.
For these patients, it would not have mattered if we had started at 0 mg morphine, 2 mg morphine, 4 mg morphine, or the larger dose of 0.1 mg/kg. There was no improvement. I know what you're thinking. At least the pain did not get worse.
How would we know? Maybe their pain did get worse, but they didn't have any higher number to use to tell us. Maybe they just initially rated their pain higher than they should have. It happens. This is one of the problems of the pain rating scale - subjectivity.

We also have too many people who feel quite comfortable under-treating the pain of other people. I do not think they should be making pain management decisions. Well, maybe they would be more appropriate making pain management decisions if they were intentionally torturing people.
If a lack of compassion/lack of empathy is a problem for healthcare providers, perhaps this is one criterion that we can use to identify those who might be better off being seamlessly integrated into the exciting field of fast food service. These paramedics, viewing patient care with a Quantity is Job One approach, will not be missed by patients. A lot of people have been saying that we should find a way to eliminate those without empathy from the classrooms. They feel that it is easier to teach people to be paramedics, than it is to teach empathy. I am not convinced, but this is certainly worth considering.
Now, let's look at the patients who were slightly better off. They only rated their pain as a 9 out of 10, initially. How did they do?
74.9% had less than a 50% relief of pain. One problem here is that half of 9 is 4 1/2. There is no 4 1/2 out of 10 on the list. Patients who started with a pain level of 9 out of 10 needed to lower it to 4 out of 10 for the purposes of it being considered a 50% decrease in pain for this study.
How would things have been different, if we split the 3 patients in half? Don't worry, when we get to the overall numbers, we end up with an even number. No procrustean methodology is intended. These 3 patients make up 25% of the patients who initially rated their pain 9 out of 10. If we split that in half, we would have 62.4% with a 50% reduction in pain. If we considered all of the 4 out of 10 patients to have had a 50% reduction in pain, then the split is 50% of the 9 out of 10 patients with a 50% reduction in pain.
The 8 out of 10 patients had 16.7% with no change in pain. A 50% reduction in pain was reported by half of the 8 out of 10 patients.
The 7 out of 10 patients had the most interesting changes. None of the patients had the same pain level as initially. 40% of the 5 patients with 7 out of 10 pain (2 patients) had an increase in level of pain. This is the kind of thing that is supposed to be impossible. Apparently, impossible is a bit over-rated.
How could a patient receive such a large dose, at least compared with what has been considered the normal dosing, and not only not improve, but have an increase in pain? Not just one patient, but 2 patients.
There is always the possibility of drug diversion, but during a study, with more people paying attention to what is going on, that is even less likely than under normal circumstances.
The 7 out of 10 patients had the worst improvement of all. Some had their pain increase, but none of them had a more than 50% improvement in their pain. Zero.
If you were to use the same approach as with the 9 out of 10 patients and count a change to 4 out of 10 as a 50% improvement, since there is no 3 1/2 out of 10, you would still have 80% with less than 50% improvement.
Finally, there are the 6 out of 10 patients. Both improved to 4 out of 10, which means none of them had more than 50% improvement in their pain.
Overall, more than 2/3 of severe pain patients had a less than 50% improvement in pain. Even if you added in the patients who improved to 5 out of 10 from 9 out of 10 and the patient who improved to 4 out of 10 from 7 out of 10, you only end up with 63.9% improving by less than 50%. Just under 2/3.
The primary measure of adequate analgesic response to morphine is percentage of reduction in pain intensity dichotomized into less than 50% versus greater than 50%. Although there are other measures, we chose a 50% or greater reduction in pain because this threshold has been used frequently in pain meta-analyses and has the appeal of quantitative simplicity and easy clinical interpretation. Patients’ age, sex, and pain location were obtained from the medical record or the patient. Ethnicity was self-reported. Additional administration of analgesics was ascertained from the records and consultation with the ED staff. Patients in this study were placed near the physicians’ and nurses’ station, directly in the line of sight of the staff and thus were under constant supervision. The research associates monitored the patients carefully as well. Vital signs were routinely measured by the nursing staff at 0, 15, and 30 minutes. For the purposes of the study, the research associates monitored the oxygen saturation, blood pressure, pulse rate, and respiratory rate at 0 and 30 minutes. Patients were reassessed by the clinical staff if systolic blood pressure was less than 100 mm Hg, pulse rate was less than 60 beats/min, or respiratory rate was less than 12 breaths/min to determine whether an opioid antagonist was needed. If oxygen saturation dropped by more than 5%, the patient was reassessed, and oxygen was administered at a fraction of inspired oxygen that returned the oxygen saturation to its baseline level. Patients whose presenting oxygen saturation was 95% or less were given oxygen on presentation.[1]
How many patients ran into problems from this larger than normal dose of morphine?
One patient was reassessed by the medical staff because the respiratory rate was 12 breaths/min, 1 patient’s oxygen saturation dropped more than 5%, 2 patients had a systolic blood pressure less than 100 mg Hg, and 8 patients had a pulse rate less than 60 beats/min (range 52 to 60 beats/min). None of the patients required administration of an opioid antagonist at any time during the 30-minute study period or for 2 hours thereafter.[1]
Not any problems that required any kind of intervention that could not be handled by a basic EMT, never mind a medic with all sorts of advanced implements of destruction. Essentially, with 10 minutes of training and authorization to add oxygen, people from registration and housekeeping could have manged these patients safely.
The protocol specified a dose of 0.1 mg/kg morphine to be given intravenously during 1 to 2 minutes. Because of rounding up or down, some patients received weight-based doses that varied slightly from the specified dose. Before data analysis, we decided to accept weight-based doses ranging from 0.09 to 0.11 mg/kg as meeting the protocol criterion for a 0.1 mg/kg standardized dose.[1]
Earlier, I mentioned that a decrease in pain to a level of 3 out of 10 is commonly used. In this study of severe acute pain, there was a less than 50% decrease in the pain level for 67% of patients.
What if the goal had been a reduction of pain to 3 out of 10, rather than the easier to reach reduction of 50%?
82% of patients did not reach the 3 out of 10 pain level.
An 82% failure rate when the goal is a pain level of 3 out of 10, or better.
A 67% failure rate when the goal is a 50% decrease in pain, or better.
People continue to tell me that this is not a problem. However, these people are not the patients with severe pain. These people are the administrators, the medical directors, the nurses, and other paramedics. In other words, the people denying the problem are the ones supposed to be making sure that this problem does not happen.
Things are improving, but it would be difficult for things not to improve. A lot of this improvement is due to research. This dismal starting point I attribute to the paranoia of the What if . . . ? crowd. They would rather restrict something they do not understand, than learn how to use it properly. They are very dangerous. Fortunately, abundant research is pointing out the ridiculous nature of their restrictions on pain management.
LIMITATIONS
Our sample is almost entirely composed of poor, inner-city Hispanic and black patients. Given the many cultural influences perception and expression of pain, it is quite possible that prevalence of poor response to morphine in other settings and other populations may differ from what we have reported. Because a convenience sample was recruited when trained research associates were present, the findings might have differed if consecutive patients had been enrolled. The patients in this study had heterogeneous locations of pain, having in common only high pain intensity and need for opioid analgesics. However, this reflects the true variety of clinical emergency practice. Some of the pain, though severe, was episodic and fluctuating. Thus, assessment of it at 30 minutes using a single numeric rating scale reading may not provide an accurate overall reflection of the degree of pain relief experienced during the preceding half hour. There is no a priori reason, however, to postulate that this methodology of sampling produces bias because pain that is changing over time seems about as likely to worsen as it does to improve throughout a constant interval.[1]
Pain of 3 out of 10 is often used, because this is a decrease to mild pain, rather than severe or moderate pain. There is much more that can be said about the ways of measuring pain, but I am not going to do that, today.
This study assessed an initial dose of morphine that is consistent with starting doses recommended in standard texts.6-8[1]
This dose clearly provides inadequate analgesia, and it may well be higher than what is routinely administered in many EDs.[1]
To summarize. 0.1 mg/kg should only be viewed as a starting dose.
Some of you may be wondering why I am using a study of morphine administered by doctors in an ED as a surrogate for morphine/fentanyl administered by paramedics before arriving at the hospital. The paramedic is as close to the patient as you are to the computer screen. How does a competent paramedic miss significant changes in patient presentation under those circumstances? There are incompetent paramedics. They should be remediated, but if they are not capable of providing competent care, they need to explore areas of employment where their lack of competence is less dangerous. There is no obligation by any employer to endanger patients by protecting the jobs of less than competent paramedics.
In the hospital, the doctors and nurses are assessing and treating other patients, documenting patient care, restocking, dealing with other patients, et cetera. If anyone believes that there is closer observation in the ED, than in a competently staffed ambulance, please provide some evidence to support this extraordinary claim.
Patients in this study were placed near the physicians’ and nurses’ station, directly in the line of sight of the staff and thus were under constant supervision.[1]
That may seem reasonable to someone who has never set foot in the Montefiore Medical Center's ED. This is not meant as a sleight to anyone working there. There are times when all sorts of craziness is going on and the claim that, without some staff member directly assigned to their care, any patients thus were under constant supervision, is not believable. In EMS, we almost always have more providers than patients. In the ED, the reverse is true. This is unavoidable.
The quote actually states, Patients in this study were placed near the physicians’ and nurses’ station, directly in the line of sight of the staff. That leads up to a conclusion that is inappropriately drawn from the first part of the sentence. The conclusion should be that because patients were directly in the line of sight of the staff, if the staff actually did look up and did focus their eyes on the patients directly in their line of sight and did decide to assess the appearance of those patients, then the patients could be said to be thus under occasional intermittent supervision at a distance. To claim that these patients thus were under constant supervision, is an unreasonably optimistic exaggeration.
Footnotes:
^ 1 Public Perception of Pain Management
Rogue Medic
Article
^ 2 Intravenous morphine at 0.1 mg/kg is not effective for controlling severe acute pain in the majority of patients.
Bijur PE, Kenny MK, Gallagher EJ.
Ann Emerg Med. 2005 Oct;46(4):362-7.
PMID: 16187470 [PubMed - indexed for MEDLINE]
^ 3 The diposi tion of morphine in surgical patients.
Berkowitz BA, Ngai SH, Yang JC, Hempstead J, Spector S.
Clin Pharmacol Ther. 1975 Jun;17(6):629-35.
PMID: 1139854 [PubMed - indexed for MEDLINE]
The disposition of serum morphine following administration of 10 mg/70 kg was determined by a sensitive and specific radioimmunoassay in 31 anethetized surgical patients ranging in age from 23 to 75 yr. Following iv injection, 93 per cent of the morphine disappeared from the serum within 5 min. The early serum levels of the drug (2 min) correlated directly with the patients' ages (r equal to 0.63, p smaller than 0.01). Patient 23 to 50 yr of age averaged 0.29 mug/ml, whereas patients 51 to 75 ur of age averaged 70 percent higher, 0.49 mug/ml. The serum half-life between 10 and 240 min was independent of age and averaged about 2 hr after either iv or im administration. Following im admininstration, morphine was rapidly absorbed, with peak levels occurring within 10 to 20 min. The decline in morphine serum levels paralleled the decline in morphine analgesia and was coincident with the apperance of morphine glucuronide in the serum. These studies demonstrate the applicability and specificity of the radioimmunoassay for morphine and suggest that serum levels of morphine may be a useful and objective indicator of its pharmacologic activity.
^ 4 Kinetics of intravenous and intramuscular morphine.
Stanski DR, Greenblatt DJ, Lowenstein E.
Clin Pharmacol Ther. 1978 Jul;24(1):52-9.
PMID: 657720 [PubMed - indexed for MEDLINE]
The disposition of parenteral morphine was assessed in two pharmacokinetic studies. In Study 1, 10 mg of morphine sulfate was administered by intravenous (IV) infusion, intramuscular (IM) injection, or both, to 8 healthy young adult male volunteers. Plasma morphine concentrations were determined by radioimmunoassay in multiple blood samples drawn after each dose. Mean (+/-SE) kinetic parameters following IV morphine were: volume of distribution (Vd), 3.2 (+/- 0.3) L/kg; elimination half-life (t1/2beta), 2.9 (+/- 0.5) hr; clearance, 14.7 (+/- 0.9) ml/min/kg; extraction ratio, 0.70 (+/- 0.04). After IM morphine, peak plasma levels ranged from 51 to 62 ng/ml and were reached within 20 min of injection. The absorption half-life averaged 7.7 (+/- 1.6) min. Systemic availability was 100% complete. In study 2, 4 elderly male patients (61 to 80 yr of age) received 45 to 80 mg of morphine sulfate IV prior to operative repair of an abdominal aortic aneurysm. Morphine pharmacokinetics were determined as described above. Kinetic variables were Vd, 4.7 (+/- 0.2) L/kg; t1/2beta, 4.5 (+/- 0.3) hr; clearance, 12.4 (+/- 1.2) ml/min/kg; extraction ratio, 0.59 (+/- 0.05). Both studies demonstrate that morphine distribution is rapid and extensive and its t1/2beta relatively short. IM morphine is rapidly and completely absorbed.
.


















